[ad_1]
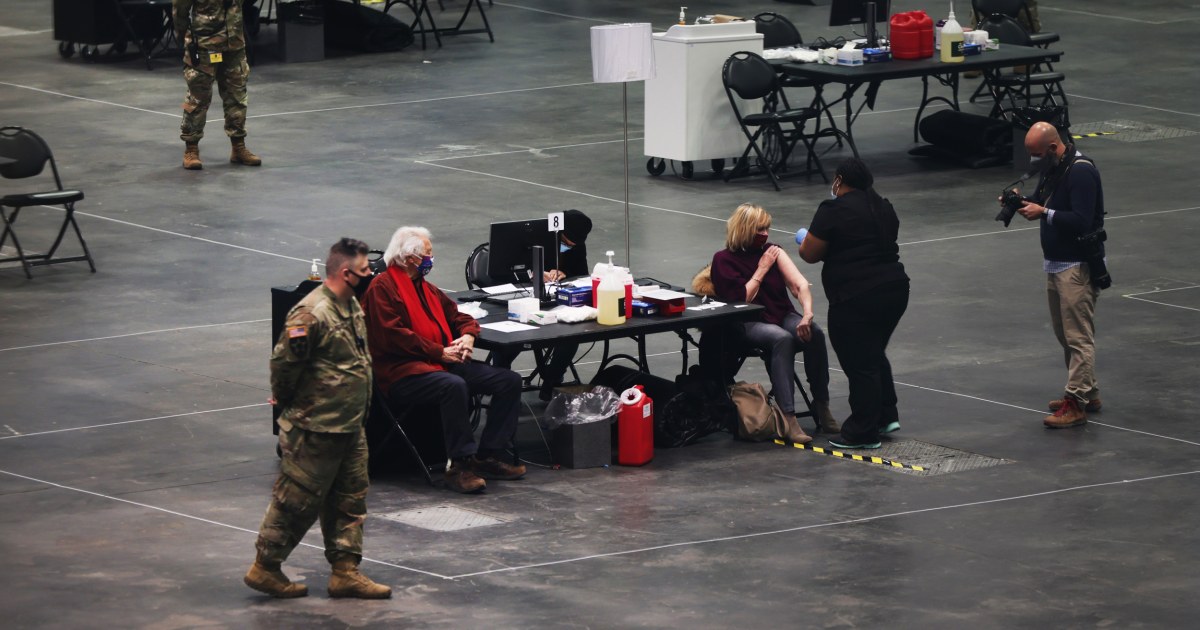
White women over 50 accounted for the majority of early Covid-19 vaccinations administered in the United States, the Centers for Disease Control and Prevention reported on Monday.
While most healthcare workers and those living in long-term care facilities are women – groups initially recommended being the first to get the vaccine – report highlights racial and ethnic inequalities among those most affected by the Covid-19 pandemic.
Comprehensive coverage of the coronavirus outbreak
Those most at risk for infection and the most dangerous outcomes are blacks, Native Americans or Alaska Natives, and Hispanics.
Of the nearly 13 million people who received at least the first dose of the vaccine between mid-December and mid-January, 63% were women and 55% were over 50, according to the CDC report.
Lack of data
Breed information was only available for about half of those vaccinated. Of these, 60% were white. It is not known why the information is missing, but this is likely due to a lack of a demographic protocol.
“The people who distribute the vaccine do not record data on race and ethnicity,” said Dr. Marcus Plescia of the Association of State and Territory Health Officials. “People need to realize this is serious. We might need a required field to make sure it’s filled out.”
Indeed, the authors of the report wrote, “A more comprehensive report of race and ethnicity data at the provider and jurisdictional level is essential to ensure rapid detection and response to potential disparities in Covid vaccination. -19. “
Addressing these disparities has become an “urgent priority” within the Biden administration.
“To achieve equity, you have to understand the disparities that exist,” said Dr. Marcella Nunez-Smith, chair of the administration’s Covid-19 health equity working group, during a briefing by the White House Monday.
“As of January 30, we were 47 percent of ethnic race data on immunization,” she said. “Let me be clear, we cannot guarantee a fair immunization program without data to guide us.”
Part of the problem is lack of access and resources.
“Some of those communities that we most worry about being hospitalized and dying also have less access to high-speed internet” for making online vaccine appointments, said Dr. Julie Morita, executive vice president of the Robert Wood Johnson Foundation.
Morita, who also served as a former health commissioner at the Chicago Department of Public Health, added that these communities may also be limited in the transportation options needed to get to vaccination sites.
“It really helps them get there and make sure these clinics are in the right places,” she said. Without proper data to determine if the right populations are being reached, “you’re really guessing.”
Nursing home staff jump shots
A second CDC report released on Monday found large gaps in vaccination efforts between those living in long-term care facilities and those caring for residents.
Among 11,460 skilled nursing facilities with at least one vaccination clinic between mid-December and mid-January, about 78 percent of residents have been vaccinated, compared with just under 38 percent of staff.
“The lower percentage of staff vaccinated raises concerns about low coverage among a population at high risk of occupational exposure to SARS-CoV-2,” the study authors wrote, referring to the virus that causes Covid-19.
Reluctance to vaccinate in this group is not a new phenomenon, the CDC reported. During the 2017-18 influenza season, immunization coverage for staff in long-term care facilities was lower than that for healthcare workers.
More recently, a survey in October 2020 found that 37% of nurses were not convinced that a Covid-19 vaccine would be safe and effective. The unprecedented speed with which these vaccines have been developed, studied and implemented seems to be at the heart of the hesitations of this group.
Dr Robert Atmar, an infectious disease physician and professor at Baylor College of Medicine in Houston, pointed out that it is possible that staff at long-term care facilities mentioned in the CDC report have received the vaccination elsewhere. and therefore were not included in this report. special report.
Yet, he said, there is a “frustration for many of us in the health care system that those who work within the system do not have confidence in health care that they do. we provide”.
Download the NBC News app for full coverage of the outbrea coronavirusk
The Food and Drug Administration has cleared two Covid-19 vaccines for emergency use. One, from Pfizer-BioNTech, was cleared on December 11, and the other, from Moderna, was cleared a week later, on December 18.
A third vaccine maker, Johnson & Johnson, is expected to request emergency use this week.
Follow NBC HEALTH on Twitter & Facebook.
Laura strickler contributed.
[ad_2]
Source link

