[ad_1]
Two clinical trials suggest that specific antibody treatments can prevent death and hospitalizations in people with mild or moderate COVID-19 – especially those at high risk of developing serious illness.
A study found that an antibody to the coronavirus developed by Vir Biotechnology in San Francisco, Calif., And GSK, headquartered in London, reduced participants’ risk of hospitalization or death by 85%. In another trial, a cocktail of two antibodies – bamlanivimab and etesevimab, both made by Eli Lilly of Indianapolis, Indiana – reduced the risk of hospitalization and death by 87%.
The study’s results, both announced on March 10, come from randomized, placebo-controlled, double-blind clinical trials, but have not yet been published. They add to a growing body of evidence that treatments can help ward off serious illness when given early, says Derek Angus, an intensive care physician at the University of Pittsburgh in Pennsylvania.
The antibodies “appear to be incredibly effective,” he says. “I am very excited about the results of these tests.”
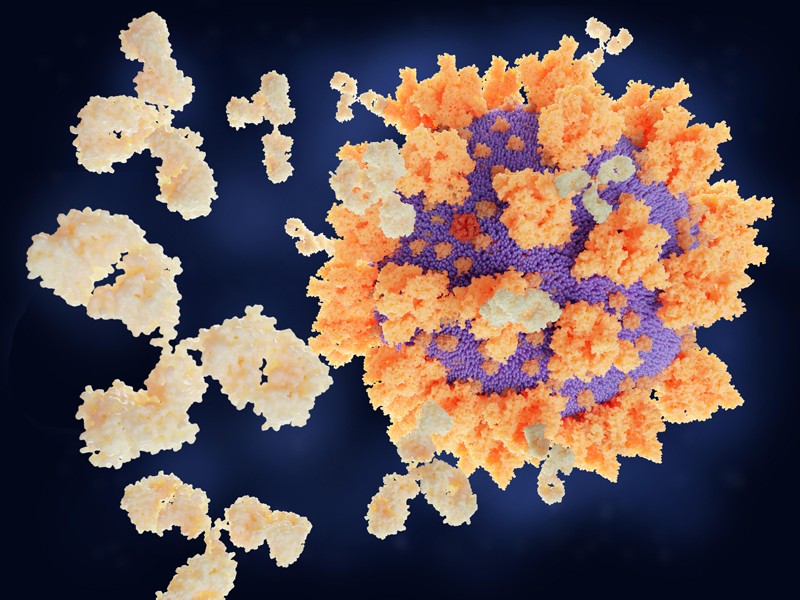
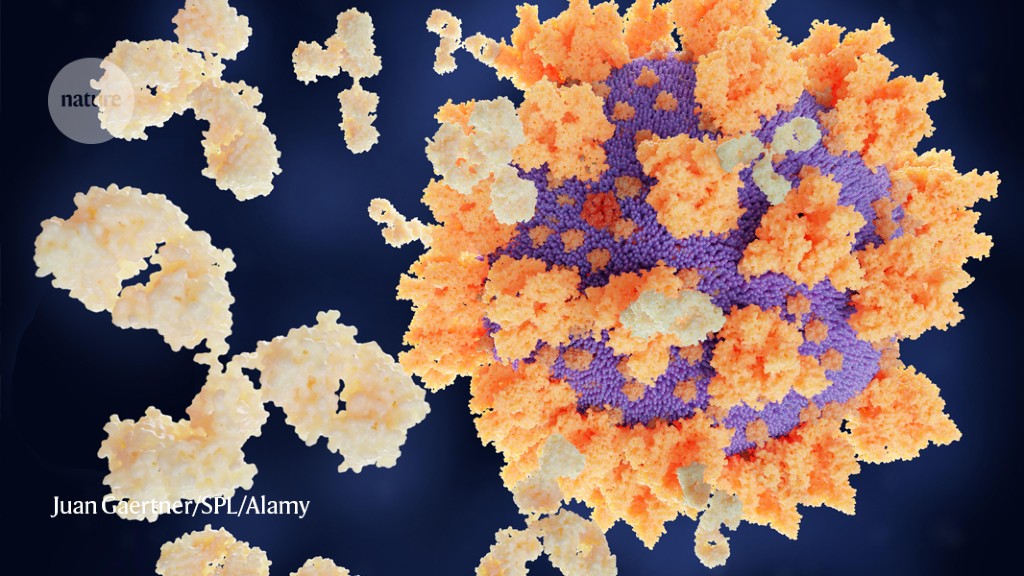
The body’s natural response to viral infection is to generate a variety of antibodies, some of which are able to directly interfere with the virus’s ability to replicate. At the start of the pandemic, researchers rushed to identify the most effective antibodies against the coronavirus and produce them in bulk. The resulting “monoclonal antibodies” have since been tested in various settings as treatments for COVID-19.
The antibody to Vir and GSK, called VIR-7831, was first isolated in 2003 from a person recovering from severe acute respiratory syndrome (SARS), caused by a similar coronavirus. The antibody was later found to bind to the SARS-CoV-2 “spike” protein as well.
The companies also announced that in laboratory studies1, VIR-7831 linked to variants of SARS-CoV-2 – including the rapidly spreading variant 501Y.V2 (also referred to as B.1.351) first identified in South Africa. They attributed the resilience of the antibody to its target: a particular region of the spike protein that does not tend to accumulate mutations.
Low absorption
VIR-7831 joins a list of monoclonal antibodies that have been tested against COVID-19, some of which – including Lilly’s combination – have already been cleared for use in the United States and elsewhere. But American doctors and their patients have been relatively unadopted, Angus says.
One problem, he says, is that although the results have been published in the press and submitted to the United States Food and Drug Administration, the companies have yet to publish data from key clinical trials in journals. with reading committee. Medicines are also expensive and must be administered by infusion in a specialized facility, such as a hospital or outpatient treatment center – a difficult task when medical resources have already been strained by an increase in cases.
Another challenge has been mixed messaging. Earlier in the pandemic, some key clinical trials involving people who had been hospitalized with COVID-19 found no benefit from monoclonal antibodies. Many researchers had anticipated this result: Monoclonal antibody therapy is expected to work best early in the disease, and late-stage symptoms of severe COVID-19 are sometimes more due to the immune system itself than it is. ‘to the virus.
Even so, these clinical trial failures created a narrative that competed with positive results in studies of milder infections, Angus says, fueling skepticism. “People were like, ‘But I thought it wasn’t working,’ he says. “It’s totally embarrassing.”
And although the studies on mild infections have shown promise, they are too small to allow researchers to draw firm conclusions, says Saye Khoo, a pharmacologist at the University of Liverpool, UK, who heads the Initiative. UK drug testing agency for the AGILE coronavirus. Only a small fraction of people with mild COVID-19 will progress to severe illness, meaning that although the trials recruited hundreds of participants, the number of those who were hospitalized or died was low.
But it will be a long wait until everyone is vaccinated, and monoclonal antibodies could be an important bridge between vaccines and treatments that have been found for people in hospital, says infectious disease physician Jens Lundgren. at the University of Copenhagen and Rigshospitalet. “It’s not a vaccine replacement, but it’s a plan B,” he says, adding that the drugs could be especially important for those who cannot mount an immune response to the vaccination.
The speed with which these monoclonal antibodies have been developed is a lesson for future pandemics, Khoo says. “These compounds are definitely exciting,” he says. “We must not forget this, because there will be other pandemics to come. It was a real lesson in how to prepare.
[ad_2]
Source link