[ad_1]
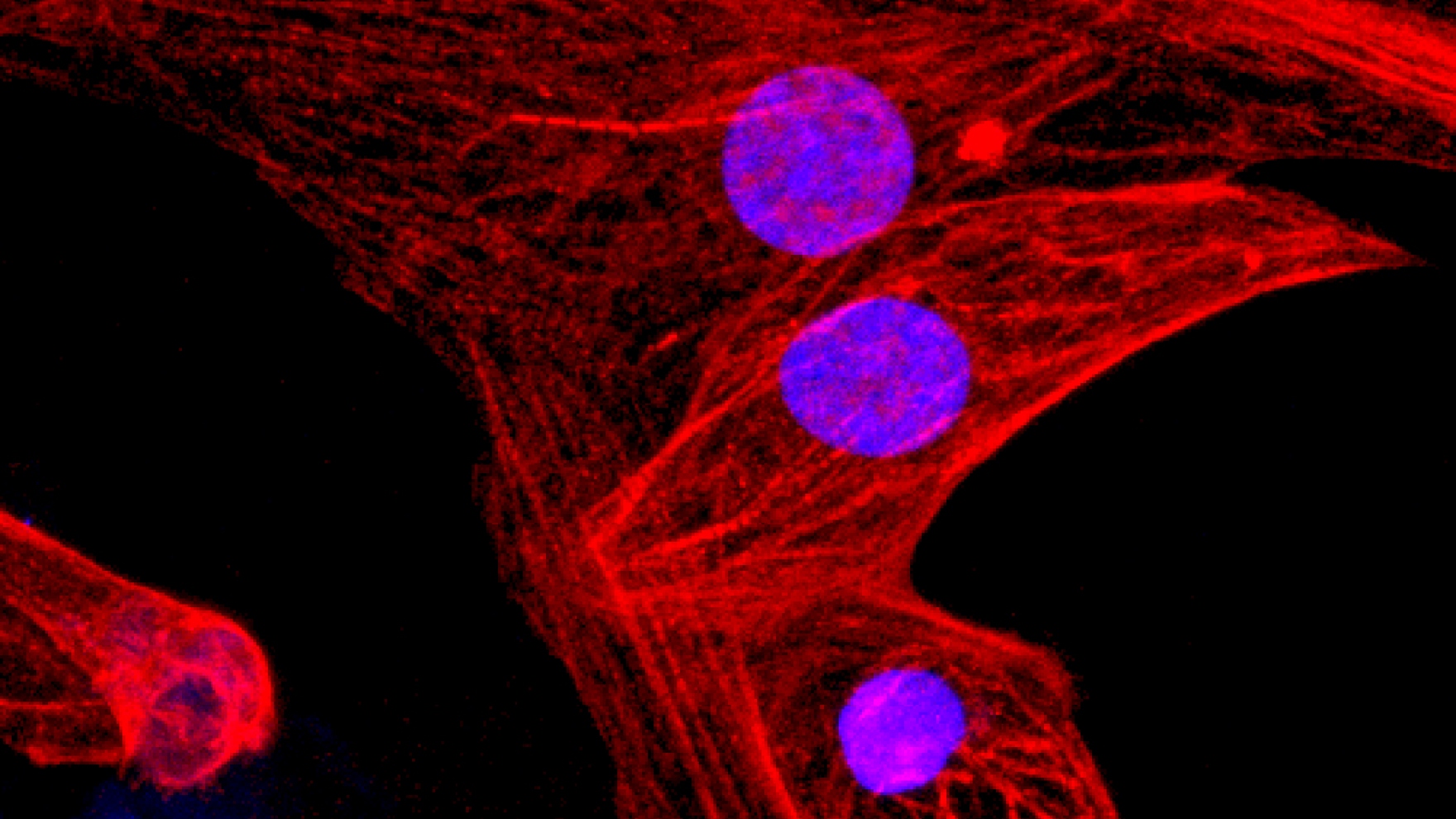
Scientists at the University of San Francisco used the CRISPR-Cas9 gene editing system to create the first pluripotent stem cells functionally "invisible" to the immune system, a feat of biological engineering that, in laboratory studies, prevented the rejection of stem cell transplants. Because these "universal" stem cells can be made more efficiently than custom-made stem cells for each patient – the individualized approach that has dominated previous efforts – they bring the promise of regenerative medicine closer to reality.
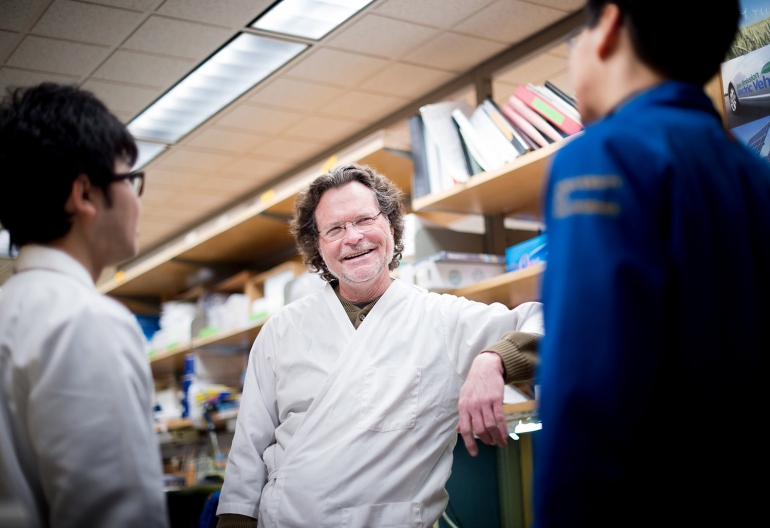
"Scientists often tout the therapeutic potential of pluripotent stem cells, which can be transformed into any adult tissue, but the immune system is a major obstacle to safe and effective stem cell therapies," Tobias Deuse said. , MD, Julien IE Hoffman, MD, Chair of UCSF Cardiac Surgery and Lead Author of the New Study, published Feb. 18 in the journal Nature Biotechnology.
The immune system does not forgive. He is programmed to eradicate everything he perceives as alien, which protects the body from infectious agents and other invaders that could wreak havoc if left unattended. But it also means that organs, tissues or grafted cells are perceived as a potentially dangerous foreign incursion, which invariably causes a vigorous immune response leading to rejection of the graft. When this happens, the donor and the recipient are told – in medical language – "incompatible histocompatibility".

"We can administer drugs that suppress immune activity and make rejection less likely. Unfortunately, these immunosuppressants make patients more vulnerable to infection and cancer, "said Dr. Sonja Schrepfer, MD, Ph.D., lead author of the study and director of the UCSF Transplantation and Immunobiology Laboratory. stem cells at the time of the study.
In the field of stem cell transplants, scientists have already thought that the problem of rejection is solved by induced pluripotent stem cells (iPSCs), created from fully mature cells – such as skin or fat cells – that are reprogrammed in order to allow them to develop. in one of the myriad of cells that make up the tissues and organs of the body. If cells derived from iPSCs were transplanted to the same patient as the original donor, the reasoning would be that the organism would perceive the transplanted cells as "self" and would not trigger the cells. immune attack.
But in practice, the clinical use of iPSCs has proven difficult. For reasons that are still unknown, many patient cells do not lend themselves to reprogramming. In addition, it is expensive and time consuming to produce iPSCs for each patient likely to benefit from stem cell therapy.
"IPSC technology poses many challenges, but quality control and reproducibility are the biggest hurdles. We do not know what makes some cells susceptible to reprogramming, but most scientists agree that it's impossible to do so reliably, "said Deuse. "Most approaches to individualized iPSC therapies have been discontinued for this reason."
Deuse and Schrepfer wondered if it would be possible to get around these difficulties by creating "universal" CSPIs that can be used by any patient in need. In their new article, they describe how, after modifying the activity of only three genes, iPSCs were able to avoid rejection after transplantation into histocompatibility-incompatible recipients with fully functioning immune systems.
"This is the first time anyone has genetically modified cells that can be universally transplanted and can survive in immunocompetent recipients without triggering an immune response," said Deuse.
The researchers first used CRISPR to remove two genes essential for the proper functioning of a class I and II major histocompatibility complex (MHC) protein family. MHC proteins lie on the surface of almost every cell and display molecular signals that help the immune system distinguish an intruder from a native. Cells lacking MHC genes do not display these signals, so they are not recorded as foreign. However, cells lacking MHC proteins become targets of immune cells called NK (Natural Killer) cells.
In collaboration with Professor Lewis Lanier, PhD – co-author of the study, director of the Department of Microbiology and Immunology of the UCSF and expert of the signals that activate and inhibit the activity NK cells – Schrepfer's team discovered that CD47, a cell surface protein acting as "Do not eat me" signal against immune cells called macrophages, also has a potent inhibitory effect on NK cells.
Convinced that CD47 could be the solution to completely suppress the rejection, the researchers charged the CD47 gene in a virus, which provided additional copies of the gene in mouse and human stem cells in which the MHC proteins had been neutralized.
CD47 has indeed turned out to be the missing piece of the puzzle. When the researchers transplanted their triple engineered mouse stem cells into mice that were incompatible with a normal immune system, they observed no rejection. They then transplanted human stem cells in the same way into so-called humanized mice – mice whose immune systems have been replaced by components of the human immune system to mimic human immunity – and again, they do not. Observed no rejection.
In addition, researchers derived various types of human cardiac cells from these triple engineered stem cells, which they transplanted again into humanized mice. Stem cell-derived cardiac cells have been able to ensure their long-term survival and have even begun to form rudimentary blood vessels and cardiac muscle, suggesting the possibility that triple-engineered stem cells may be used someday to repair failing hearts.
"Our technique solves the problem of rejection of stem cells and stem cell-derived tissue and represents a major breakthrough in the field of stem cell therapy," said Deuse. "Our technique can benefit more people with lower production costs than any individualized approach. We only need to make our cells once and we end up with a product that can be applied universally. "
authors: Other authors include Xiaomeng Hu (co-first author), Alessia Gravina, Dong Wang and Grigol Tediashvili from UCSF, the University Heart Center in Hamburg, the Cardiovascular Research Center in Hamburg and the German Center for Cardiovascular Research; Victor J. Garcia of the University of North Carolina School of Medicine; and Mark M. Davis of Stanford University and Howard Hughes Medical Institute. Lewis Lanier is Professor of the American Cancer Society and Director of the Department of Microbiology and Immunology; J. Michael Bishop, MD, Distinguished Professor of Microbiology and Immunology; and director of the Parker Institute for Cancer Immunotherapy at UCSF.
Funding: The research was funded by grants from the Deutsche Forschungsgemeinschaft, the Leducq Foundation, the Max Kade Foundation, the California Institute of Regenerative Medicine, the National Institutes of Health and the Parker Institute for Cancer Immunotherapy.
Conflicts: The authors declare a lack of financial interests in competition.
UC San Francisco (UCSF) is a leading university dedicated to promoting health worldwide through advanced biomedical research, graduate training in life sciences and professions of health and excellence of patient care. It includes leading graduate schools in dentistry, medicine, nursing and pharmacy; a graduate-level division with nationally-recognized programs in the basic, biomedical, translational and demographic sciences; and a leading biomedical research company. It also includes UCSF Health, which includes three leading hospitals – the UCSF Medical Center and UCSF Benioff Children's Hospitals in San Francisco and Oakland – as well as the Langley Porter Hospital and Psychiatric Clinics, UCSF Benioff Children's Physicians. and the cabinets of the UCSF. UCSF Health has affiliations with hospitals and health organizations throughout the Bay Area. The UCSF faculty also provides all medical care provided to the public at the San Francisco Zuckerberg General Hospital and Trauma Center, as well as at SF VA Medical Center. The UCSF Fresno Medical Education Program is a major branch of the Faculty of Medicine at the University of California, San Francisco.
[ad_2]
Source link