[ad_1]
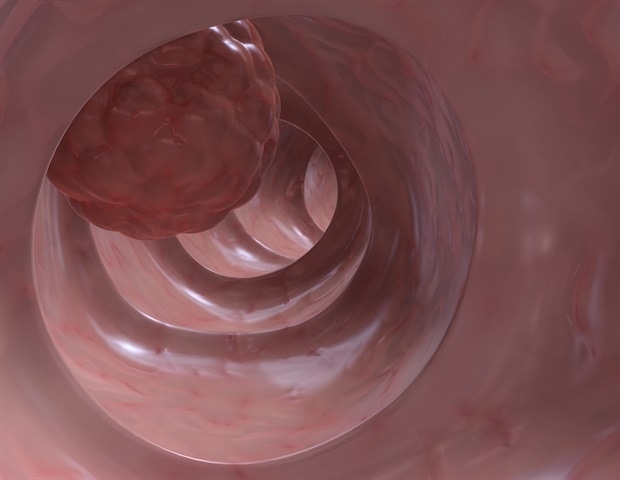
Advanced colon cancer often spreads on a large scale and may not respond to standard chemotherapy. In such a case, a new combination of drugs and a flexible dosage can help to get better prospects, as shown by several new studies.
In one study, researchers explored the use of paclitaxel in the treatment of metastatic squamous cell carcinoma of the anus. A combination of 5-fluorouracil (5-FU) and cisplatin is the current first-line treatment for metastatic disease, but there is no standard treatment for refractory tumors (resistant to standard treatment). In this scenario, 6 patients were treated with paclitaxel, used in similar tumors of the head and neck. Weekly treatment with paclitaxel resulted in a measurable response in 4 patients, while another showed stabilization of the disease after this treatment.
The results of the European REARRANGE trial were presented at the 2018 ESMO World Congress on Gastrointestinal Cancer. They involved nearly 300 patients in Spain, Italy and France. These patients were on average 64 years old and all had refractory metastatic colorectal cancer (MCR). All had progressed from first-line treatment to fourth-line treatment.
Regorafenib is a multi-kinase inhibitor used in refractory coronary coronary cancers, but with an excessively high rate of discontinuation due to serious adverse effects. The purpose of the trial was to evaluate the effect of dosing changes on the safety, toxicity, and overall survival of this drug.
Patients were randomly badigned to one of three groups: standard dose (SD), dose reduction (DR) and intermittent dose (ID). SD patients received 160 mg / day, while RD patients took 120 mg / day, both for three weeks followed by one week of rest. In the ID group, regorafenib 160 mg / day was used over one week.
If cycle 1 of RD and DI treatment was well tolerated, all patients were switched to the DS cycle. Guillem Agiles, author of the study, explains: "We reduced the dose during the first cycle and then increased because it was shown that the toxicity was higher during the first and second months of treatment."
Although the total number of grade 3 or 4 adverse events did not change, the use of RD and ID in the first few months was numerically badociated with a reduction in the number of adverse events. number of adverse events leading to discontinuation of treatment, such as fatigue, hypertension and hand-foot skin reaction. (HFSR) Treatment duration and median progression-free survival (approximately 3-4 months and 2 months respectively) were not affected, making it a viable alternative. more important so far in this area, so has supported the use of flexible dosage of regorafenib in this state.
Agiles explains: "These results, interpreted in the context of other trials, such as the US ReDOS study (3), indicate that the more flexible doses of regorafenib are an effective alternative to improve the quality of life of patients. refractory metastatic patients. Other oncologists have also been impressed. "Eric Van Cutsem, a professor at the University of Leuven, predicted that this would change the way that regorafenib is used in the treatment of cancer mCRC.
The ESMO congress has also heard of another major breakthrough: the BEACON CRC study on a combination of three drugs used to treat refractory mCRC carriers with the BRAF V600E mutation. This mutation is observed in 15% of patients with mCRC and has a poor prognosis.
The trial was conducted in 665 patients in three treatment groups: triplet treatment with encorafenib, binimetinib and cetuximab; doublet treatment with encorafenib and cetuximab; and one of two chemotherapeutic regimens (irinotecan or combination of folinic acid, fluoruracil and irinotecan (FOLFIRI) with cetuximab).
The triplet combination of non-chemotherapeutic agents has been developed to suppress both the BRAF kinase pathway and other compensatory mechanisms allowing tumor cells to develop resistance to BRAF inhibitors. Scott Kopetz, author of the study, commented: "Colorectal cancer does not respond to treatment with BRAF alone, because tumor cells adapt by other mechanisms after the initial treatment. With this triple targeted therapy, we use a very scientifically logical combination to inhibit BRAF and these other mechanisms. "
Triplet treatment was well tolerated and resulted in a median overall survival of 9 months and an objective response rate of 26% versus 5.4 months and 2%, respectively, with standard therapy. This remarkable improvement has forced an expert to stress the need for routine BRAF testing in all patients with CRC, making it the new standard of care. "We now have a specific treatment that can change the natural course of the disease in patients with BRAF mutations and that is better than the previous treatment, so it is essential that patients undergo routine tests," said the professor. Andres Cervantes of Valencia.
In addition, avoiding chemotherapy is a big bonus. Cervantes said, "In many other types of cancer, and particularly in colorectal cancer, it is common for targeted biologic therapies to be used in combination with chemotherapy. The fact that we can give this targeted combination without the need for chemotherapy is very good news for patients, especially because of the side effects they usually experience with chemotherapy. "
Although only refractory patients with metastatic colorectal cancer who have failed up to two lines of chemotherapy are currently eligible for this treatment, it should be studied in other BRAF mutant tumors, whether in prior cancer cancer or adjuvant therapy following primary excision of the tumor rates.
The last word? Modifying drug combinations and regimens promises to improve the lives of mCRC patients while maintaining treatment efficacy.
sources:
Journal reference:
K Rekai, Belkharoubi K, Larbaoui B, P-001, Paclitaxel for the treatment of bad cancer after cisplatin and 5-fluorouracil, Annals of Oncology, Vol. 30, Supplement No. 4, July 2019, mdz155, https: // doi .org / 10.1093 / announce / mdz155
[ad_2]
Source link