.jpg)
[ad_1]
Amid the 2019 coronavirus disease pandemic (COVID-19), some groups are observed to be at a higher risk of developing serious illness. These include the elderly, the immunocompromised, and those with underlying health conditions, such as diabetes, hypertension, kidney disease, obesity, and heart problems.
One of the conditions linked to an increased risk of death from COVID-19 is diabetes, a condition characterized by high glucose levels in the body.
.jpg)
Researchers at Xijing Hospital, Fourth Military Medical University, Xi’an, China, have found that diabetes and admission glucose levels may increase the risk of death from COVID-19.
Diabetes and COVID-19
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to spread around the world, with the number of confirmed cases reaching nearly 100 million.
Although lower than previous coronavirus outbreaks, COVID-19 has a death rate of around 1-5%. Most of the reported deaths are in older adults and people with co-morbidities.
Previous reports have shown that diabetes has a 2: 3 risk ratio for mortality. Moreover, in China, the China Center for Disease Control and Prevention reported that among more than 72,000 patients with COVID-19, diabetics had a death rate of 7.3%, compared with 2.3% in the general infected population.
Besides COVID-19, people with diabetes are also at higher risk for other infections. Previous studies have shown that glucose levels are associated with an increased risk of being admitted to hospital for infections in general, including respiratory tract infections.
Meanwhile, previous reports have shown diabetes to be one of the most common comorbidities in patients with COVID-19.
Diabetic patients with COVID-19 may have a poor prognosis, as evidenced by the fact that the incidence of diabetes was twice as high in ICU / severe cases as in their non-ICU / severe counterparts, ”explained l ‘team.
The study
The study, published on the pre-print medRxiv * server, investigated 2,877 patients, who were admitted to Huo Shen Shen Hospital, dedicated solely to treating COVID-19 in Wuhan City, the original epicenter of the coronavirus pandemic in December 2019.
Overall, the study found that admission blood sugar was associated with later mortality.
To arrive at the study results, the team investigated the association of diabetes, admission glucose, and antidiabetic drugs with mortality or death from COVID-19.
Researchers found that among patients hospitalized for COVID-19, 39 died in hospital and 387 had a history of diabetes. Compared to the 40 patients who survived, the deceased patients were older and had a higher prevalence of comorbidities such as hypertension, diabetes, previous surgery, and myocardial angina or chest pain.
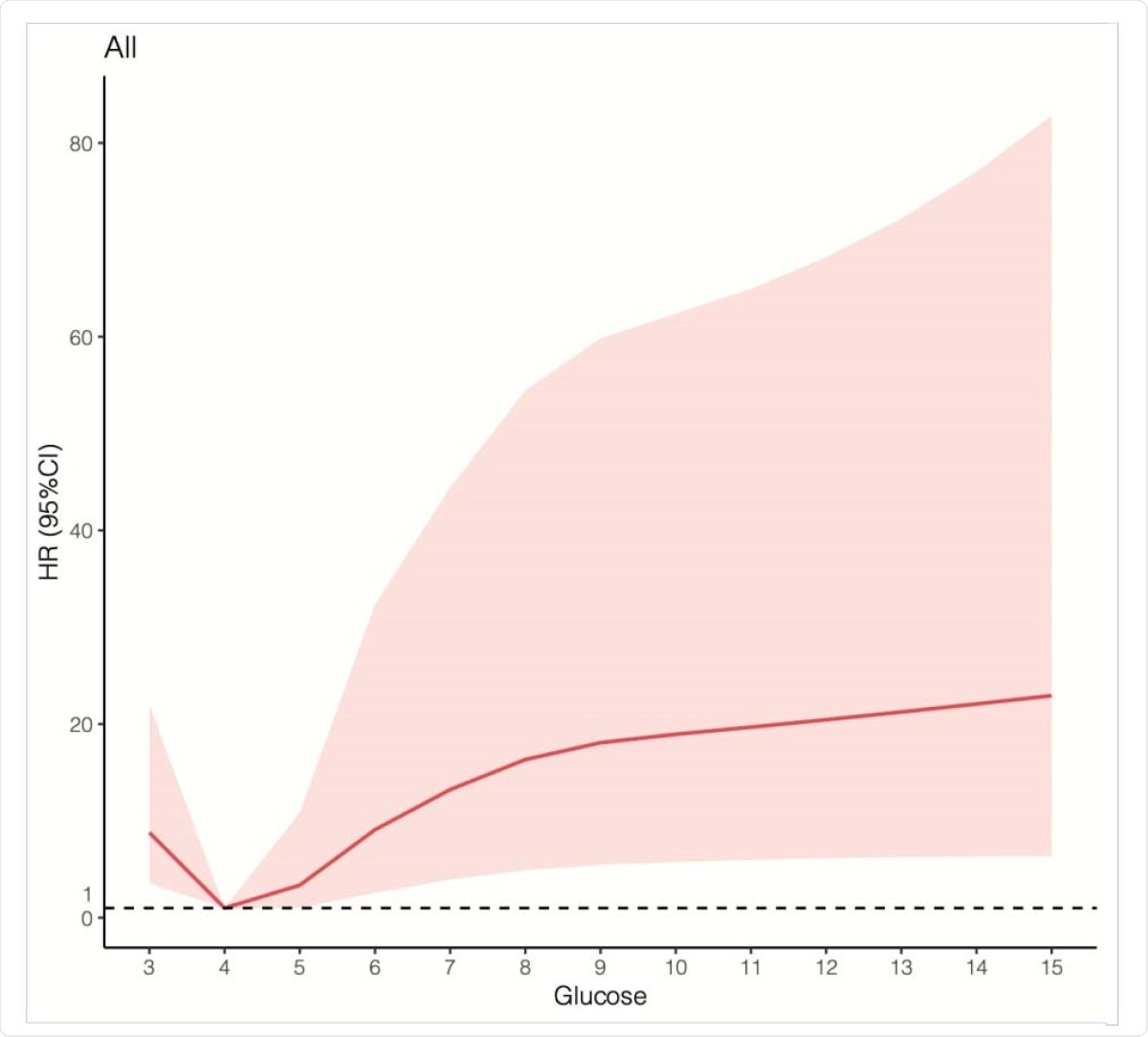
Association between glucose and mortality risk ratio in an adjusted cubic spline of 33 in 34 patients with COVID-19.
Additionally, people who died had a higher respiratory rate and were more likely to experience difficulty breathing.
Overall, the researchers noted that diabetes was independently linked to increased mortality. They recommend that regular blood sugar monitoring can reduce the risk of developing severe symptoms.
Diabetes and admission blood sugar (per mmol / L ≥ 4 mmol / L) are associated with increased mortality in patients with COVID-19. These data support that blood sugar must be properly controlled for possibly better survival results in patients with COVID-19, ”the team concluded.
*Important Notice
medRxiv publishes preliminary scientific reports which are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or treated as established information.
Source:
Journal reference:
Source link