[ad_1]
A study recently published in the journal parish described a case report of a patient with coronavirus 2019 (COVID-19) who presented with pneumonia, posterior reversible encephalopathy syndrome (PRES) and persistent cortical blindness. A detailed clinical presentation of the patient is provided in the report.
Context
Since the emergence of the COVID-19 pandemic caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), several studies have been conducted to identify specific signs and symptoms as well as adverse complications associated with the disease. In addition to pulmonary and cardiovascular difficulties, patients with severe COVID-19 have been shown to have neurological complications, including headache, dizziness, encephalopathy, delirium, meningitis, encephalitis, acute transverse myelitis, and smell and taste disturbances. Against this background, studies have shown that neurological complications associated with COVID-19 are primarily caused by direct viral invasion and inflammation in the neural network.
In the current case report, scientists described the clinical consequences of a 54-year-old COVID-19 patient who presented with SARS-CoV-2-related pneumonia, posterior reversible encephalopathy syndrome (PRES) and blindness persistent cortical.
Important observations
The patient’s initial clinical presentations were fever, dry cough, and myalgia for ten days, in addition to severe shortness of breath. At the time of hospitalization, the patient had an elevated body temperature, a significantly elevated heart rate, and an oxygen saturation level of 82%. Due to a further deterioration in the patient’s state of health, non-invasive ventilation was implemented.
According to clinical examinations, the patient had lower levels of lymphocytes in the blood; however, no abnormalities in renal function, electrolyte balance, and blood coagulation profile were observed. Based on the chest x-ray observation of bi-basal union and a respiratory swab specimen positive for SARS-CoV-2, the patient was empirically administered amoxicillin / clavulanic acid and clarithromycin.
Due to increased oxygen demand, the patient was subjected to endotracheal intubation and mechanical ventilation after ten days of admission. After further examinations, the patient was diagnosed with acute respiratory distress syndrome and systemic inflammatory response syndrome. Based on the clinical profile of the patient, a possibility of sepsis could not be excluded and, therefore, treatment with broad-spectrum antibiotics was initiated. Throughout the hospital stay, the patient did not receive any steroids or immunomodulatory drugs.
On day 21, the patient had a generalized seizure and a brain CT scan was performed, which suggested the possibility of PRES. Although the patient gradually stabilized and mechanical ventilation was withdrawn, neurological examination revealed the presence of complete cortical blindness and Anton syndrome (denial of vision loss). Although the patient began to recognize shapes and colors due to progressive physical and neurological recovery, a significant level of visual impairment persisted.
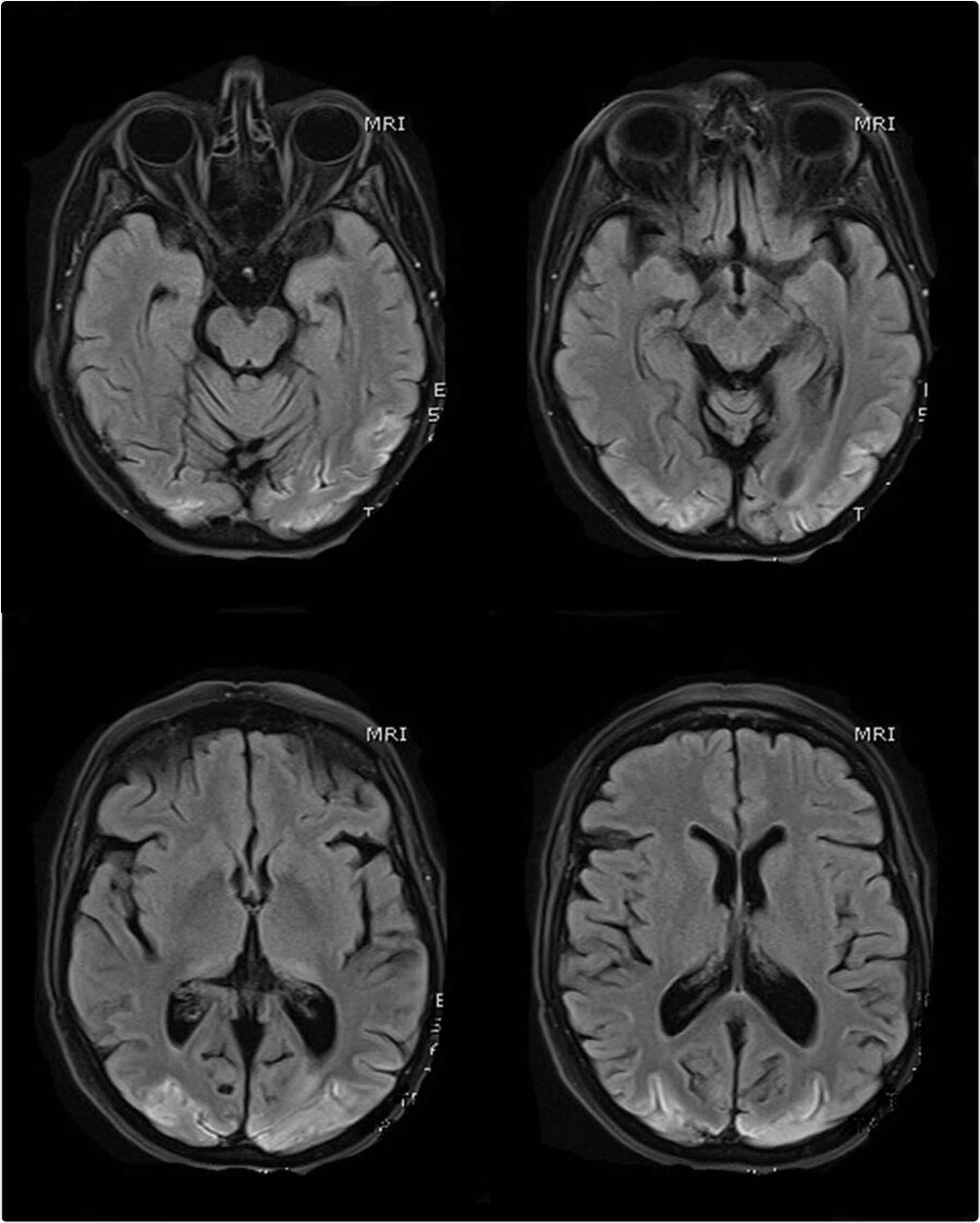
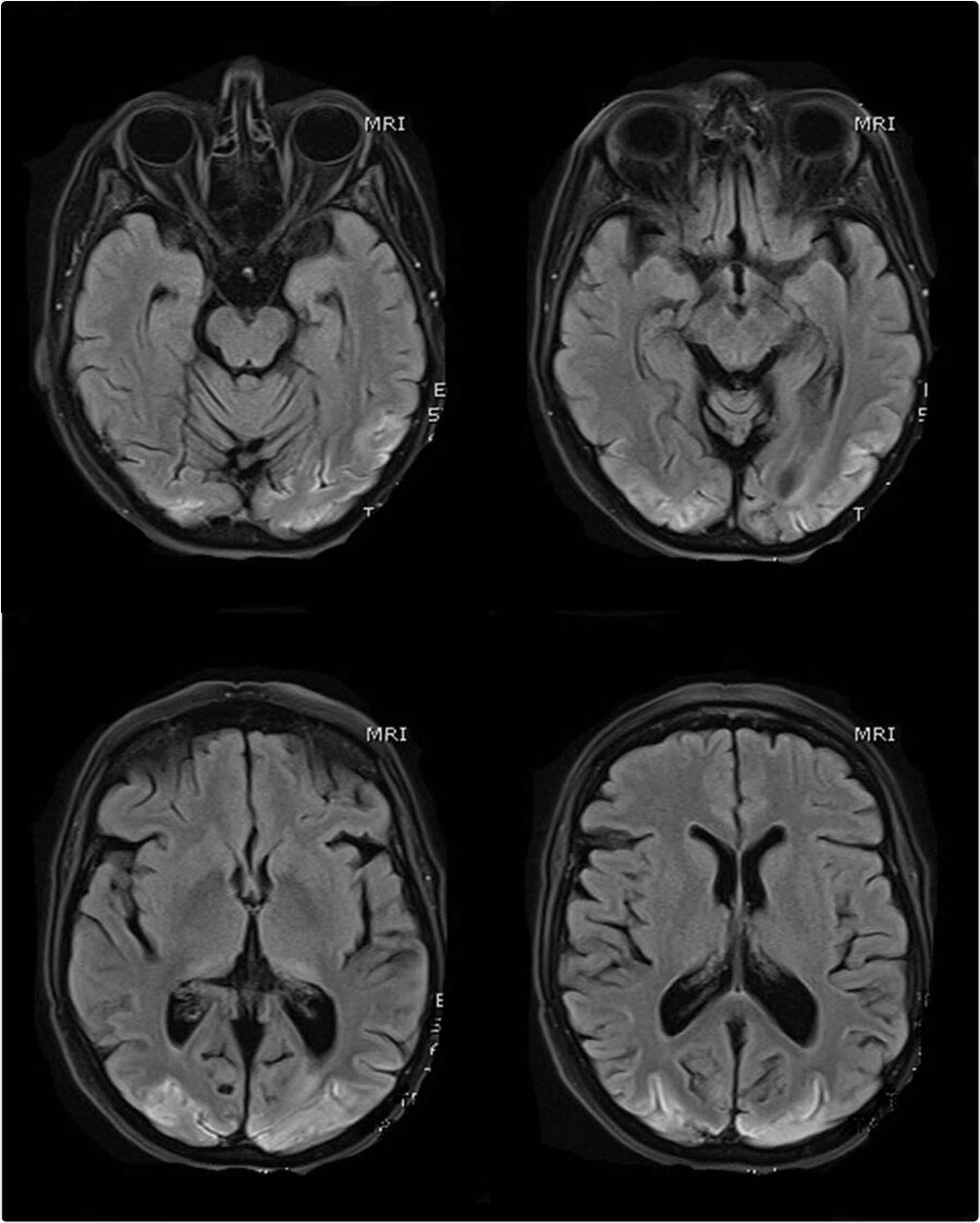
MRI scans of the brain (selected T1 sequences) show bilateral symmetrical hyperintensity involving the bilateral occipital lobe cortex; changes correspond to pseudolaminar cortical necrosis as a complication of posterior reversible encephalopathy syndrome (PRES)
The importance
According to the available literature, cerebral hyperperfusion caused by hypertension is a significant risk factor for PRES. Thus, the authors suggest that tight regulation of blood pressure is essential for COVID-19 patients to avoid the risk of PRES, which is otherwise a rarely seen SARS-CoV-2 complication. However, in the current study, the patient’s highest blood pressure was 190/90 mmHg right after the first attack. Otherwise, the patient displayed normal blood pressure throughout his hospital stay. Therefore, the authors suggest that high blood pressure is not the main reason for PRES in this case.
Because sepsis was suspected, the authors suggest that endothelial dysfunction linked to COVID-19 could be a potential cause of PRES.
Taken together, the authors suggest that PRES, along with persistent cortical blindness, should be considered one of the rare complications associated with SARS-CoV-2 infection.
Source
Source link