[ad_1]
As the 2019 coronavirus disease (COVID-19) pandemic crosses grim milestone of over one hundred million reported cases, the rollout of some vaccines offers a distinct silver lining that some degree of control could be achieved within a year. Now, a new, pre-printed research paper describes a chimpanzee adenovirus vector vaccine which, when administered intranasally in rhesus macaques, led to a robust immune response and demonstrated protection against infection. by the virus that causes COVID-19, namely the severe acute respiratory syndrome coronavirus. 2 (SARS-CoV-2). The pre-print is published on the bioRxiv* server.
Previous conclusions
In a previous study, the vaccine candidate demonstrated protection against upper and lower respiratory tract infection in mice expressing the viral receptor, the human angiotensin converting enzyme 2 (ACE2). The current study extended these results to show its effectiveness in non-human primates.
SARS-CoV-2 peak antigen
The virus enters the host cell via the engagement of its spike antigen with the cell surface ACE2 receptor. The spike protein (S) is therefore a critical vaccine target and central to the development of therapeutic antibodies. The S protein is cleaved in several steps, first at the S1 / S2 interface. The S1 subunit is responsible for binding to the receptor at the receptor binding domain (RBD), then in the S2 domain to produce the S2 ‘protein which mediates viral membrane-cell fusion.
Neutralizing antibodies recognize the prefusion protein S, which has RBD in its “up” conformation. Candidate vaccines under development include DNA / RNA vaccines, lipid nanoparticle-encapsulated mRNA (LNP), inactivated viral vaccines, protein subunit vaccines, and viral vector vaccines.
Inability to prevent viral spread
Most vaccines currently available and those in phase III trials require two doses and are administered intramuscularly. These conditions not only require a longer period of time for protective immunity to set in but do not confer local or mucosal immunity, allowing viral shedding to continue.
Therefore, vaccinated individuals can still transfer the infectious virus to others, even if they themselves are protected from infection. (Moderna vaccine has been shown to reduce viral shedding through the nose in laboratory animals, but human data are lacking.)
Experiments with intramuscular (IM) vaccines in non-human primates (NHPs) show that despite the protection they offer against COVID-19 pneumonia, the same cannot be said for upper airway infection and , therefore, against viral transmission.
Different vaccine antigens
The researchers described the use of the SARS-CoV-2 vaccine based on the chimpanzee adenovirus (simian Ad-36) (ChAd-SARS-CoV-2-S) which expresses the protein S. Previously, when administered intranasally to mice, a single dose elicited protective antibodies and cell-mediated immunity against the spike protein and prevented infection of the upper and lower respiratory tract.
The spike protein used in this vaccine candidate (ChAd-SARS-CoV-2-S) differs from the other Ad-23-based chimpanzee vaccine, ChAdOx1 nCoV-19, in phase III trials, in that ‘it exhibits backbone deletions which upregulate peak expression and stabilize proline mutations to maintain the protein in its pre-fusion form.
The current study used an intranasal dose of the vaccine in rhesus macaques (Macaca mulatta), followed by challenge with SARS-CoV-2 via the intranasal and intrabronchial routes.
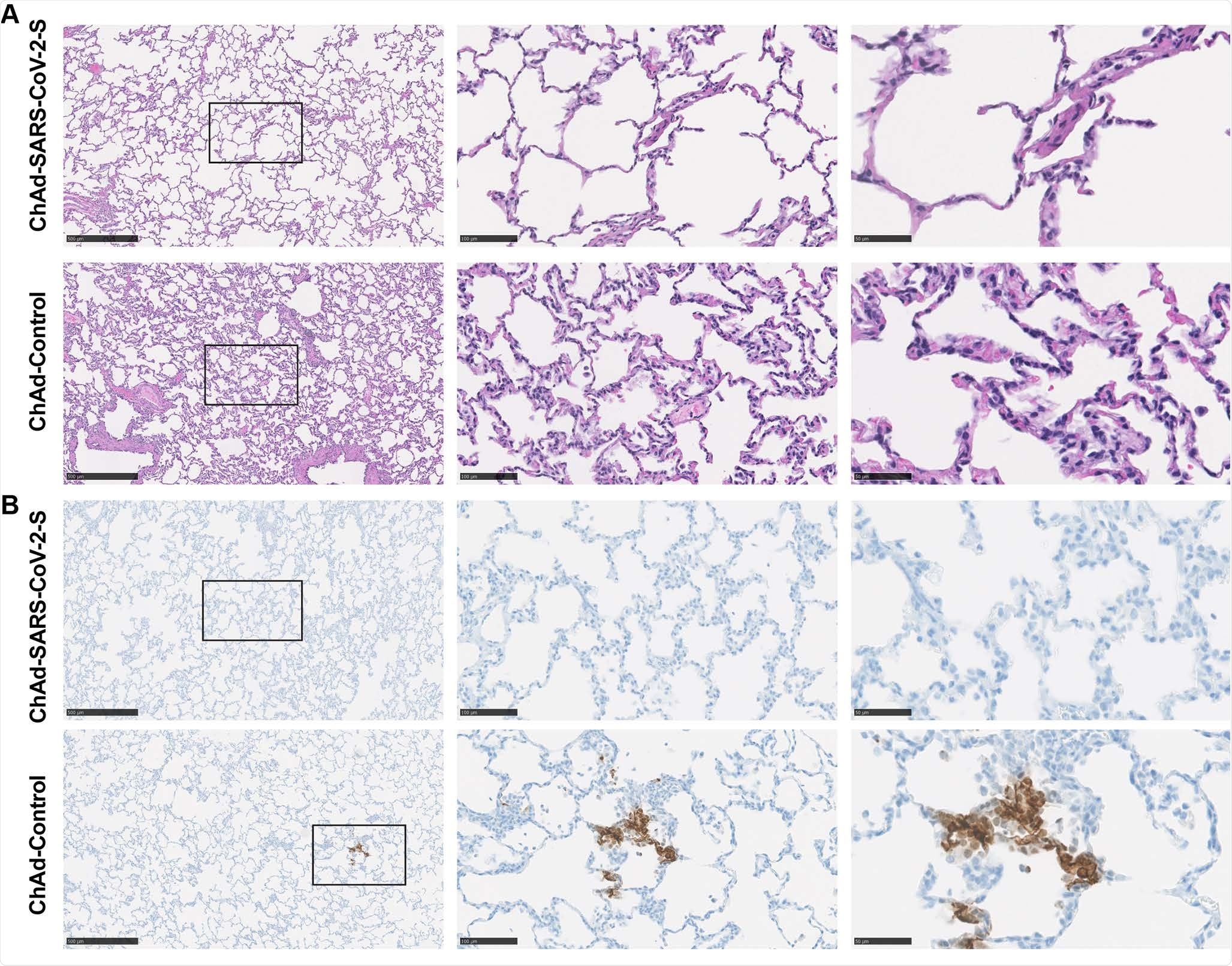
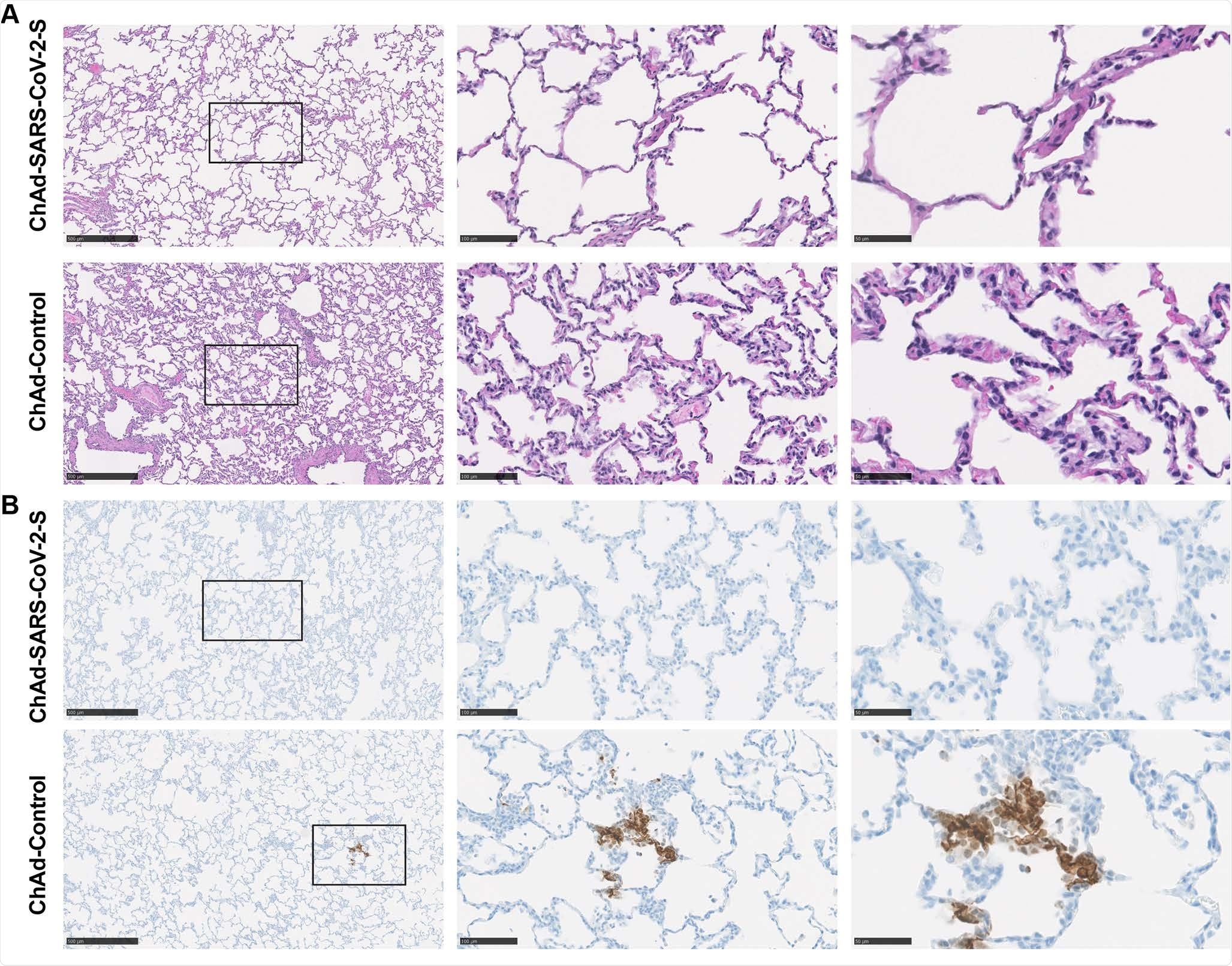
Pathological analysis of the lungs of vaccinated MRs. RMs were immunized with ChAd-control and ChAd-SARS-CoV-2-S and challenged. The lungs were harvested at 7 dpi. A. Sections were stained with hematoxylin and eosin and imaged. Each image is representative of a group of 6 RM. B. The SARS-CoV-2 antigen was detected in lung sections of MR for the conditions described in (A). Images show low (left; scale bars, 500 μm), medium (middle; scale bars, 100 μm), and high magnification (right; scale bars, 50 μm). Representative images of n = 6 RM per group.
Immunogenic vaccine
They found anti-S, anti-RBD and neutralizing antibodies. T cell responses were also present.
Protection against local infections
In nasal swabs, viral RNA loads were lowered in immunized animals, and only one had infectious virus detectable on the first day after challenge, compared to four of six controls. At later times, no infectious virus was isolated from a nasal swab.
This suggests that local infection is avoided, with lower levels of viral RNA and faster viral clearance.
Protection against lung infections
The researchers also measured the level of infection in bronchoalveolar lavage fluid (BALF) on days 1 and 3 after challenge and lung tissue (day 7), from exposed animals. One of six samples on day 1 was positive for infectious virus, compared to all control samples. The viral titer was also three orders of magnitude lower.
On day 3, a single sample from a control animal was positive for infectious virus. Viral RNA was increased 100-fold and 50-fold, on days 1 and 3, respectively, in BALF control samples compared to immunized animals, which promotes viral clearance.
Lung tissues of controls also showed a much higher level of viral RNA in immunized animals compared to day 7 controls. In fact, the higher the titer of neutralizing antibody, the higher the BALF viral RNA was. low. This correlation was more sensitive than that of anti-S IgG, indicating that the titer of neutralizing antibody may be proportional to the level of protection offered by this vaccine.
Staining of viral antigen in the lungs of immunized animals was absent, compared to four of six control animals.
What are the implications?
Both at the point of entry and in distant tissues, a single dose of ChAd-SARS-CoV-2-S vaccine could dramatically reduce disease incidence and viral spread. Of course, there was a low incidence of severe pulmonary pathology, or disease, in both control and immune animals, despite the use of high doses of infection and the introduction of infectious virus by the intranasal and intrabronchial routes. . This limits any conclusion about the protective efficacy of this vaccine against the disease induced by SARS-CoV-2.
“As this single intranasal dose vaccine confers protection against SARS-CoV-2 in non-human primates, it is a promising candidate for limiting the infection and transmission of SARS-CoV-2 in humans.“Further research could focus on ways to increase the extent of protection, including the potential use of a homologous or heterologous booster dose with the same vaccine or another adenovirus vector vaccine.
Another encouraging sign is the lack of increase in vaccine-dependent disease. However, more research is needed to compare the immunity achieved with intranasal and IM administration of this vaccine, as well as the timescale of immunity over time after intranasal vaccination with ChAd-SARS-CoV-. 2-S.
*Important Notice
bioRxiv publishes preliminary scientific reports which are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or treated as established information.
Source
Source link