[ad_1]
Gaining more fat cells probably isn’t what most people want, although it might be exactly what they need to fight diabetes and other illnesses. How and where the body can add fat cells has remained a mystery – but two new studies from UT Southwestern provide answers on how this process works.
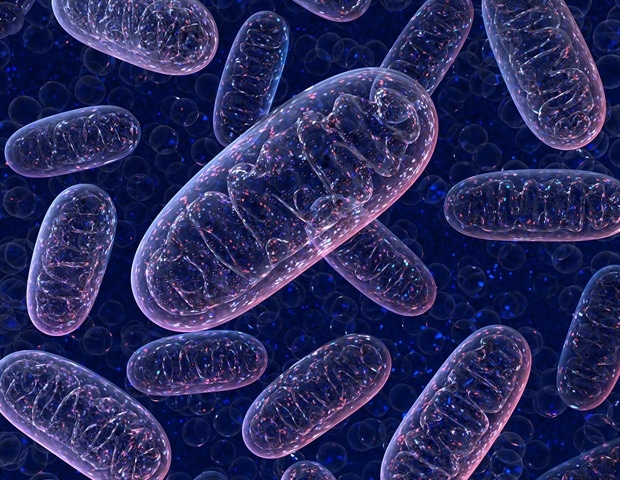
The studies, both published online today in Cell stem cell, describe two different processes that affect the generation of new fat cells. One of them reports how the creation of fat cells is affected by the activity level of tiny organelles inside cells called mitochondria. The other describes a process that prevents new fat cells from growing in a fat storage area in mice – the area that correlates with healthy subcutaneous fat just under the skin in humans. (Both studies were performed in mice.)
In the second study, a commonly used anticancer drug was able to jumpstart the creation of healthy fat cells in mice, a finding that raises the possibility of future drug treatments for humans.
While fat isn’t popular, as long as people eat too much, they’ll need a place to store excess calories, says Philipp Scherer, Ph.D., director of the Touchstone Center for Diabetes Research at UT Southwestern and lead author of the first study. focusing on the mitochondria.
There are two options, he says: squeezing more lipids (fat) into existing fat cells and inflating their size, leading to problems such as inflammation and, eventually, diabetes; or by creating new fat cells to help distribute the load. Fat stored properly – in layers of fat cells under the skin (subcutaneous fat) that aren’t overloaded instead around organs (visceral fat) or even inside organs – is the healthy alternative, says -he.
Problems arise if existing fat cells are left on their own to become engorged, adds Rana Gupta, Ph.D., associate professor of internal medicine and lead author of the second study. “When these cells are so overwhelmed that they can’t take it anymore, they eventually die or become dysfunctional, dumping lipids into places not intended to store fat.
These lipids can enter the liver, causing fatty liver disease; to the pancreas, resulting in diabetes; or even to the heart, causing cardiovascular disease, Gupta says. Visceral or abdominal fat can surround organs, creating inflammation.
The healthiest place to store fat is in subcutaneous fat, Gupta adds. Ironically, this is where the mice in his study were least able to create new fat cells, despite the fact that stem cell-like progenitor cells, ready to become fat cells, were also present there, says- he.
Gupta’s study identified a process that prevents progenitor cells from developing into fat cells in the subcutaneous inguinal fat of mice.
The HIF-1a protein (short for hypoxia-inducible factor 1 alpha) is at the heart of the process. It triggers a series of cellular actions that ultimately inactivate a second protein called PPARgamma, the main driver of fat cell formation.
These proteins are found in both humans and mice. In fact, in a culture of human subcutaneous fat cell progenitors, HIF-1a also inhibited the creation of new fat cells, according to Gupta.
In Gupta’s study in mice, researchers used a genetic approach to inhibit HIF-1a and found that progenitor cells could then produce subcutaneous inguinal fat cells and less were inflamed or fibrous.
Then they tested the cancer drug imatinib (brand name Gleevec) and found that it had the same effect. The anti-cancer drug was tried because it was known to have diabetes benefits in cancer patients with both diseases, Gupta says.
In Scherer’s study, researchers manipulated a protein called MitoNEET in the outer membrane of the mitochondria of precursor cells, organelles called the powerhouses of cells. The resulting mitochondrial dysfunction and decreased cell metabolism caused precursor cells to lose the ability to become new fat cells and increased inflammation.
This study shows that we can manipulate the willingness of precursor cells to become fat cells. The ability to recruit new fat cells by tickling these pre-fat cells to become fat cells is very important and has profound health benefits, especially in the obesity-prone environment in which we are. let’s all live. “
Philipp Scherer, Ph.D., Director, Touchstone Center for Diabetes Research, UT Southwestern
He says his goal now is to design a drug that could stimulate mitochondrial activity.
“Understanding the mechanism is an important first step,” says Scherer, referring to the results of the two studies. “We will have to learn in the future how to manipulate these processes pharmacologically.”
Source:
UT Southwestern Medical Center
Source link