
[ad_1]
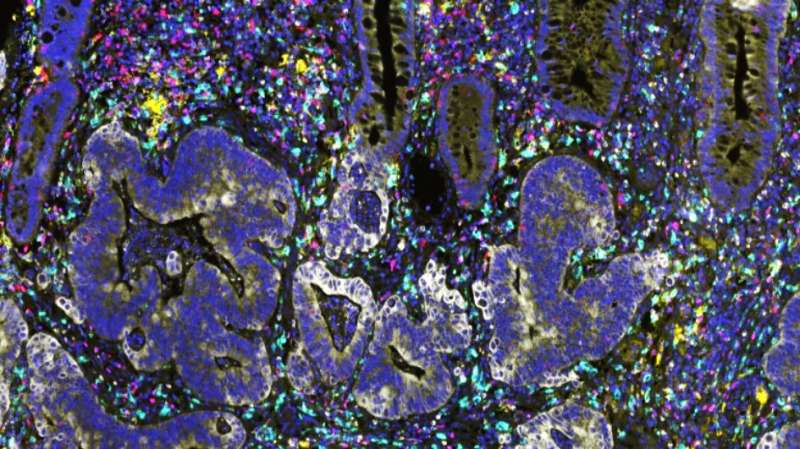
Colored intestinal tumor section. Credit: Dr David Mansfield, Senior Scientific Officer at ICR
Cancers resistant to radiation therapy could be made susceptible with immunotherapy treatment, a new study suggests.
Manipulating bowel cancers according to their “immune landscape” could open up new ways of treating resistant tumors.
Cancers can change resistance to radiation therapy just as they do with drugs.
The new study found that profiling the immune landscape of cancers before treatment could identify patients who may respond to radiation therapy early on, and others who may benefit from priming their tumors with immunotherapy.
Inflammation predicts response to radiation therapy
Scientists at the Institute of Cancer Research in London, in collaboration with the University of Leeds and the Francis Crick Institute, studied inflammation in samples of intestinal tumors taken before and after radiation therapy in 53 patients. They aimed to understand how the immune activity of tumors before and after radiation therapy differs between patients who respond well and those who respond poorly to treatment.
The study is published in the Journal for Cancer Immunotherapy and was supported by the NIHR Biomedical Research Center at the Royal Marsden NHS Foundation Trust, ICR and the Medical Research Council.
The team showed that the effectiveness of radiation therapy depends in part on the level of inflammation within the tumors before and after treatment.
In the study, patients who showed poor response to radiation therapy – without a substantial drop in tumor cell count – started with chronically inflamed tumors, with high levels of activity in 40 immune genes. The level of inflammation in their tumors showed minimal changes after radiation therapy.
In contrast, the good responders – who saw a marked drop in tumor cell count during radiation therapy – started with a relatively weak inflammatory tumor landscape that accelerated after treatment. Here, there was a significant increase in the activity of 198 immune genes, including genes representing immune cells that can directly kill tumor cells.
Careful synchronization of immunotherapy alongside radiation therapy could unblock resistant cancers
Taken together, the results show that carefully planning a combination of immunotherapy and radiation therapy, based on an assessment of the cancer immune landscape, could provide a way forward for treating resistant cancers.
Although the study was conducted specifically in bowel cancer, the researchers believe the findings might be relevant for other types of disease as well, particularly for cancers where surgery is not an option and radiotherapy is particularly important.
A growing body of evidence shows that radiation therapy works not only by causing DNA damage and cell death in cancer cells, but also in a potentially vaccine-like manner – triggering the immune system to recognize cells. tumors and speed up an immune response to attack them.
This work is part of a growing activity at ICR and in radiotherapy and immunology that includes the RadNet radiotherapy research network, in collaboration with The Royal Marsden.
Immunotherapy and Radiation Therapy Could Be a Very Powerful Mix
Study leader Dr Anguraj Sadanandam, head of the ICR Systems and Precision Cancer Medicine team, said:
“Radiation therapy has revolutionized cancer treatment and is the most effective way to cure cancer other than surgery.
“Our study showed that the immune landscape and levels of inflammation in cancers are critical in determining how they respond to radiation therapy. This suggests that the combination of radiation therapy and immunotherapy could turn out to be a very powerful mixture. – improving our ability to eliminate hard-to-treat cancers.
“We now wish to improve our understanding of how to combine and sequence radiation therapy and immunotherapy together to maximize treatment response for each patient’s individual biology.”
Study co-author Dr. Anna Wilkins, clinical researcher in the ICR Clinical Trials and Statistics Unit, now at the Francis Crick Institute, said:
“Radiation therapy is an important curative treatment option for many cancer patients. We are starting to understand why the immune response is important for radiation therapy to work most effectively.
“Our study suggests that by targeting specific non-cancerous cells that block this immune response, we may further improve radiation therapy responses in patients.”
Dr Nick West, University Clinical Research Fellow at Leeds University and Honorary Consultant in Gastrointestinal Pathology, said:
“Radiation therapy is commonly used in patients with rectal cancer and there are currently no validated biomarkers that reliably predict cancer response. Patients who do not respond well to radiation therapy may still experience significant side effects despite the lack of clinical benefit.
“This study suggests that we can potentially improve the response of these patients through modulation of the immune system, which is a very exciting development. The study also showed that a new technique developed at the University of Leeds, the tumor cell density, can be used to objectively measure the degree of tumor response to radiation therapy. “
Adjustment of the radiotherapy response using immunotherapy
Professor Paul Workman, Director General of ICR, said:
This fascinating study adds to the evidence that the effectiveness of radiation therapy is closely related to the involvement of the immune system. It is now clear that the response of radiation therapy in cancer cells and surrounding tissues may enable the immune system to a patient to recognize and destroy his tumor.
“But radiation therapy requires a healthy immune response, and the new research suggests we may need to fine-tune that response through immunotherapy. It could provide a basis for future trials to test new drug combinations, including immunotherapies alongside radiotherapy. ”
Study reveals inhibitory role of ‘Ter cells’ in cancer therapy
Anna Wilkins et al. Differential and longitudinal immune gene models associated with the reprogrammed microenvironment and viral mimicry in response to neoadjuvant radiotherapy in rectal cancer, Journal for Cancer Immunotherapy (2021). DOI: 10.1136 / jitc-2020-001717
Provided by the Cancer Research Institute
Quote: Targeted Immunotherapy Could Boost Radiation Therapy Response (2021, March 8) Retrieved March 8, 2021 from https://medicalxpress.com/news/2021-03-immunotherapy-boost-radiotherapy-response.html
This document is subject to copyright. Other than fair use for private study or research purposes, no part may be reproduced without written permission. The content is provided for information only.
[ad_2]
Source link