[ad_1]
Chimeric antigen receptor T cell therapy, or CAR T, is a relatively new type of therapy approved for treating several types of aggressive B cell leukemia and lymphoma. Many patients react strongly to CAR T; however, some have only a short response and quickly develop disease progression. Unfortunately, it is not completely understood why these patients have progression. In an article published in Proceedings of the Royal Society BResearchers at the Moffitt Cancer Center are using mathematical modeling to explain why CAR T cells work in some patients and not in others.
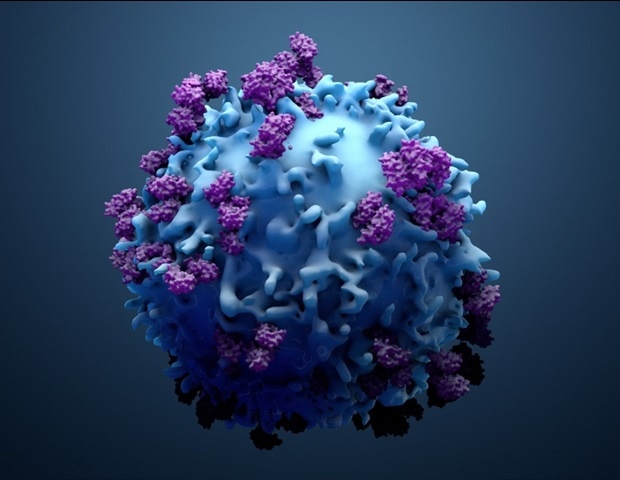
CAR T is a type of personalized immunotherapy that uses a patient’s own T cells to target cancer cells. T cells are harvested from a patient and genetically engineered in a lab to add a specific receptor that targets cancer cells. The patient then undergoes lymphodepletion with chemotherapy to lower some of their existing normal immune cells to help the expansion of CAR T cells which are injected back into the patient, where they can go to work and attack the tumor.
Mathematical modeling has been used to help predict how CAR T cells will behave after being re-injected into patients; however, no study has yet examined how interactions between normal T cells and CAR T cells impact the dynamics of therapy, particularly how nonlinear T cell kinetics play a role in the odds of therapy success. . Moffitt researchers integrated clinical data with mathematical and statistical modeling to address these unknown factors.
Researchers demonstrate that CAR T cells are effective because they expand rapidly after being injected back into the patient; however, modified T cells have been shown to compete with existing normal T cells, which may limit their ability to grow.
“The success of the treatment depends primarily on the ability of the CAR T cells to multiply in the patient, and this directly depends on the effectiveness of lymphodepletion which reduces normal T cells before the infusion of CAR T,” said Frederick Locke. , MD, co-lead author of the study and vice chair of the department of blood and bone marrow transplantation and cell immunotherapy at Moffitt.
In their model, the researchers found that tumor eradication is a random event, but potentially highly probable. Despite this randomness of cure, the authors demonstrated that the differences in timing and likelihood of recovery are largely determined by the variability between patients and the factors of the disease. The model confirmed that healings tend to occur early, within 20 to 80 days of the decline in CAR T cell numbers, while disease progression tends to occur over a wider range of time between 200 and 500 days after treatment.
The researchers’ model could also be used to test new treatments or come up with sophisticated clinical trial designs. For example, the researchers used their model to demonstrate that another round of CAR T cell therapy would require a second lymphodepletion with chemotherapy to improve patient outcomes.
“Our model confirms the hypothesis that sufficient lymphodepletion is an important factor in determining a sustainable response. Improving the adaptation of CAR T cells to grow further and survive longer in vivo could lead to an increase the likelihood and duration of response, ”said Philipp Altrock, PhD, lead author of the study and associate member of Moffitt’s Integrated Mathematical Oncology Department.
Source:
H. Lee Moffitt Cancer Center & Research Institute
Source link