[ad_1]
Amphotericin, an antifungal agent capable of puncturing holes in cell membranes, could replace broken ion channels in the lung tissue of patients with cystic fibrosis.1 Tests conducted on cell cultures and pigs designed to display the symptoms of the disease have shown that the compound restores the lung's ability to release bicarbonate, which is essential for the functioning of the organ. The team behind the work is now pushing for clinical trials.
Cystic fibrosis (CF) affects one in 2,500 newborns and is caused by a genetic abnormality that leaves patients with breathing difficulties and chronic lung inflammation. This disease significantly reduces the life expectancy of people with Alzheimer's disease at around 47 years old.
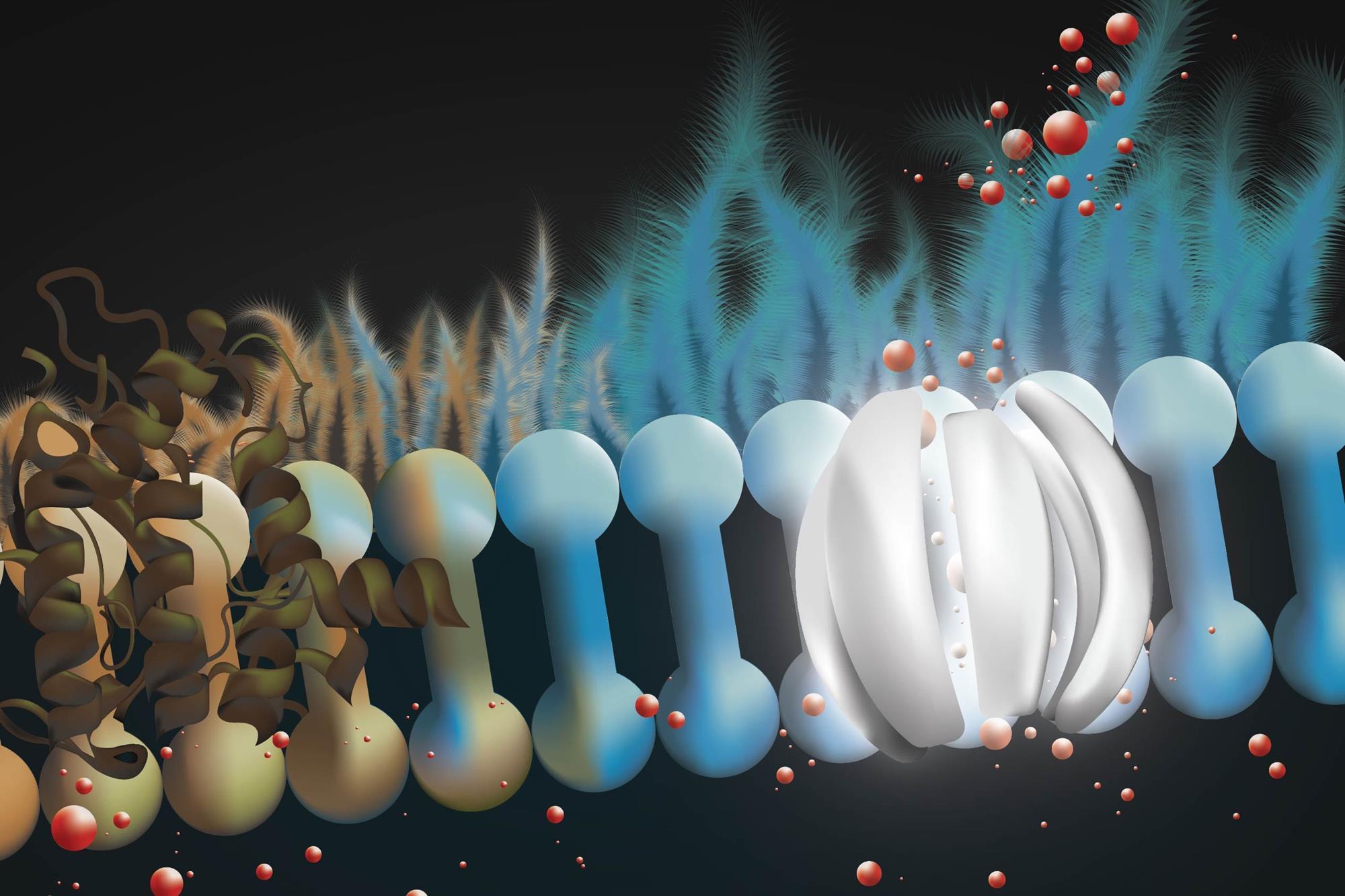
CF causes an abnormality in the CFTR protein, located in the lung membrane. It prevents cells from releasing bicarbonate and chloride ions into the liquid beneath the highest mucus layer, which then becomes thick and sticky – fertile ground for bacteria. Cystic fibrosis is not cured, although in some cases the drugs partially restore the functioning of the CFTR.
Chemist Martin Burke of the University of Illinois at Urbana – Champaign in the United States and a team of biochemists, geneticists and physicians used amphotericin B, a macrocyclic polyene-polyalcohol, as a prosthesis ion channel to replace the broken CFTR. Tests on human cell cultures and porcine models of cystic fibrosis have shown promising results: amphotericin was able to release the bicarbonate and chloride ions trapped in CF lung cells. In cell cultures, the effect lasted seven days, while animal experiments lasted only two hours.

Amphotericin has affinity for cell membranes and can pierce ion permeable holes. Scientists have long thought that this made it toxic in large doses. "In fact, that's what's written in my textbook since I was in medical school," says Burke. But it turns out that it is not true. Amphotericin kills cells by extracting sterols from their membranes. Burke's team simply pre-complexed amphotericin with sterols to prevent this.
Imperfect imitation
"Overall, it's impressive, but very surprising that it worked," said Michael Gray, researcher in cell physiology, University of Newcastle, UK. "Nobody has chosen to test a non-selective pore … others have considered using anionophores or small peptides, but nothing really substantial has come out of this work."
In terms of gross functionality, amphotericin is much simpler than CFTR. While the latter is a selective secretor of bicarbonates and chlorides, the antifungal is a non-selective channel for all monovalent ions. But that may be all that is needed to recover CF lung function.
"We've been waiting a long time for a perfect replacement of a missing protein to restore health," Burke said. "I think the most important finding of our study is that the imperfect imitation of a missing protein with a small molecule can in many cases be sufficient to restore physiology."
Burke's hypothesis is that the electrochemical gradient created by the other pumps and cell channels is enough to push the good ions through the amphotericin hole. "Other proteins can correct imperfections by pumping other ions in the other direction," he says. When the other pumps are blocked, the amphotericin becomes ineffective.
Difficult delivery
"This would be an approach for hard-to-correct CFTR mutations that would not produce functional protein in the cell membrane," said Beate Illek, director of the cystic fibrosis research laboratory at the Oakland Hospital Research Institute, in the USA. There are 2,000 different defective versions of the gene encoding CFTR. Thus, about 15% of patients do not benefit from drugs that promote CFTR protein activity, says Gray.
"However, delivering drugs into the inflamed and infected airways is problematic, and the drug has to get into the sticky mucus layer," says Illek. In their tests, Burke's team added amphotericin directly into the lungs of pigs through a tracheal window. Finally, they hope to administer it via an inhaler. "Nebulized amphotericin has already been given to people with cystic fibrosis to treat a fungal disease. In these cases, although there has been some improvement in lung function, nothing dramatic has been observed, "says Gray.2
Burke now wants to conduct clinical trials. Amphotericin is already approved as a drug against fungal infections, so he hopes to find "a very fast and safe way" to test its effectiveness.
"But as excited about the study as we are, it's really important to point out that it remains to be seen if this can be helpful for people with cystic fibrosis," Burke said.
[ad_2]
Source link