[ad_1]
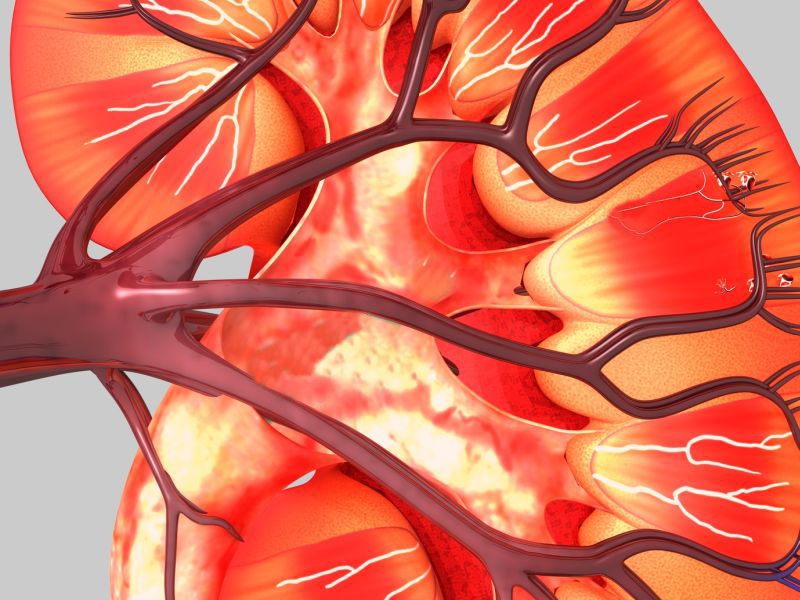
MONDAY, April 15, 2019 (HealthDay News) – A new antidiabetic drug could also significantly reduce the risk of death from kidney failure and heart disease in diabetic patients with kidney failure, a new study finds.
According to experts, information about Invokana (canagliflozin) is important because diabetes and kidney disease often go hand in hand.
"Diabetes is the leading cause of kidney failure in the world, but for nearly two decades, there have been no new treatments to protect kidney function," said the author Principal Investigator, Vlado Perkovic. He is a professor at the George Institute for Global Health of the University of Oxford in the United Kingdom.
"The final results of this trial constitute a major medical advance as people with diabetes and kidney disease are at an extremely high risk of kidney failure, heart attack, stroke and stroke. deaths, "said Perkovic in a press release issued by the university. "We now have a very effective way to reduce this risk by using a pill once a day."
The research was funded by the pharmaceutical company Janssen, which manufactures Invokana. The study involved more than 4,400 patients with diabetes and kidney disease in 34 countries. Half took Invokana and the other half a "dummy" pill against placebo. All have been treated for kidney disease according to the guidelines in force.
Those taking Invokana were 30% less likely to develop kidney failure, 30% fewer deaths from kidney failure or heart disease, 20% less likely to experience major cardiac events such as heart attack, stroke or death. Cardiac origin. , and a hospitalization risk for heart failure reduced by 39%, the researchers reported.
The results were published on April 15 in the New England Journal of Medicine.
According to the study, which was also expected to be presented Monday at the ISN World Nephrology Congress, in Melbourne, Australia, there was no risk of major side effects at home. those who had taken Invokana.
Invokana belongs to a clbad of antidiabetic drugs called glucose and sodium 2 transporter (SGLT2) inhibitors.
Meg Jardine, co-author of this study, an badociate professor at the George Institute, said: "With 5 million people worldwide who would suffer from kidney failure by 2035, it is about A major step forward. "
Two diabetes and kidney care experts who read the new study agreed that the results are significant.
"More than 40% of patients with end-stage renal failure have diabetes as a cause of their kidney failure," said Dr. Maria DeVita, chief of nephrology at Lenox Hill Hospital in New York.
She explained that SGLT2 inhibitory drugs such as Invokana work by blocking the "reuptake" of glucose into the kidneys. More sugar in the blood, as well as salt, are therefore safely excreted in the urine instead of staying in the kidneys where they can cause damage, DeVita said.
Thus, Invokana "could substantially alter the trajectory of kidney decline, preserving kidney function for years longer than we thought possible in the long term," DeVita said. "This is great news for people with diabetic nephropathy."
Dr. Guy Mintz directs cardiovascular health at the Sandra Atlas Bbad Heart Hospital in Manhbadet, NY. He also thinks the new discoveries are "exciting".
"With another impressive study of this family of drugs, SGLT2 inhibitors should now be used in all type 2 diabetic patients with renal impairment with increased cardiovascular risk", as long as it does not occur. There is no reason not to do it, says Mintz.
"This is another tool at our belt to reduce progressive kidney failure and cardiac events in our type 2 diabetic population with kidney failure," he said.
More information
The National Kidney Foundation has more about diabetes and kidney disease.
SOURCES: Maria DeVita, MD, Chief of Nephrology, Lenox Hill Hospital, New York; Guy Mintz, MD, Director, Cardiovascular Health and Lipidology, Sandra Atlas Bbad Heart Hospital, Manhbadet, N.Y .; Oxford University, press release, April 15, 2019
[ad_2]Source link