[ad_1]
A bacterial infection better known to cause gum disease can lead to the development of Alzheimer's disease in some patients by entering the brain and releasing enzymes that attack important proteins.
Cortexme scientists, working with academics around the world, say the results of their study could lead to new treatment options for people with Alzheimer's disease who target the bacteria. Porphyromonas gingivalisand have developed a drug candidate in clinical trials.
"We studied this particular pathogen because several previous studies had been published, suggesting a link between P. gingivalis and Alzheimer's disease, "says Stephen Dominy, senior scientist at Cortexis. Recent research has suggested that amyloid beta – one of the aggregates forming proteins in the brain of patients with Alzheimer's disease – was an antimicrobial peptide formed in response to bacterial infections in the brain, and P. gingivalis specifically in the brains of people with Alzheimer's disease.
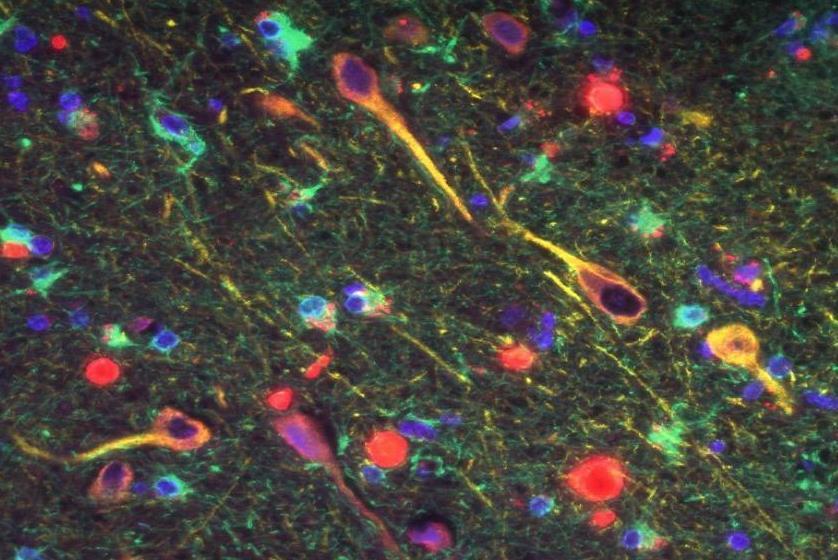
The Cortexine study examined the brain tissue of patients with Alzheimer's disease and found that more than 90% of the samples contained gingipain, the harmful enzymes secreted by P. gingivalis, with significantly higher levels in the brains of patients than in those in good health. They detected the bacterium's DNA in the cerebrospinal fluid of seven out of 10 live patients diagnosed with Alzheimer's disease.
They also showed that when genetically modified mice predisposed to Alzheimer's were infected with P. gingivalis, the bacteria found themselves in their brains and this was badociated with increased levels of amyloid protein. Gingipains have also been shown to damage Tau protein, another brain protein involved in the development of Alzheimer's disease.
"Based on these results, we believe that P. gingivalis is the leading cause of Alzheimer's disease and gingipaines are the main factors of Alzheimer's pathology, "said Dominy.
Treatment in development
P. gingivalis Infections are usually treated with antibiotics, but Dominy and his colleagues found that treating cells infected with antibiotics did not stop the damage caused by the enzymes. Instead, they developed a small molecule that inhibits the gingipans themselves, which could reduce neurodegeneration in mice injected with these enzymes. The treatment has recently successfully pbaded human safety studies and is expected to enter phase II / III clinical trials in patients with mild to moderate Alzheimer's intensity. year.
David Reynolds, Scientific Director of Alzheimer's Research UK, said that the idea that gum disease was linked to Alzheimer's disease had been circulating for several years, but that this work is "a step forward". "A few years ago, it was suggested [amyloid] Accumulation could be part of the brain's innate immune system to bacteria, "he says. "At the same time, people have tried to show that in patients with periodontal disease, their cognitive decline was progressing faster … what this study does more than any other, is to try to bring these two together. elements. "
He says that it's important to remember that the study was conducted by a company developing gingipain antagonists to treat dementia. "What this article shows is their preclinical data – or at least the parts they want to show the world – that help them strengthen their story," he says. He points out that, while most of the data presented in the study on cortexts supported their hypothesis, gingipains were not found in all brains with Alzheimer's disease. the only cause ".
He adds that although we do not yet know how much this affects the risk of dementia, "maintaining good dental health is an important part of a healthy lifestyle". Dominy agrees. "Certainly, reduce the P. gingivalis the burden in the mouth, especially at an early age, should be taken more seriously than it is currently based on our data, "he adds, although it is unlikely that the mere targeting of the disease gums contribute to the treatment of infections. P. gingivalis in the brain.
Given the failure of almost all drug trials for Alzheimer's disease, it has been suggested that the focus on beta-amyloid is misguided and may be a symptom rather than the cause. Reynolds points out that these results must be taken into account in existing research that highlights a number of factors other than bacterial infection at the heart of the development of Alzheimer's disease. "What we do not know is [whether] it's a potential cause in a sub-group of patients, or something that aggravates a pathology already under way, "he says. "Clearly, clinical trials will help to understand this in more detail."
[ad_2]
Source link