[ad_1]
Editor’s Note: Find the latest COVID-19 news and advice in Medscape’s Coronavirus Resource Center.
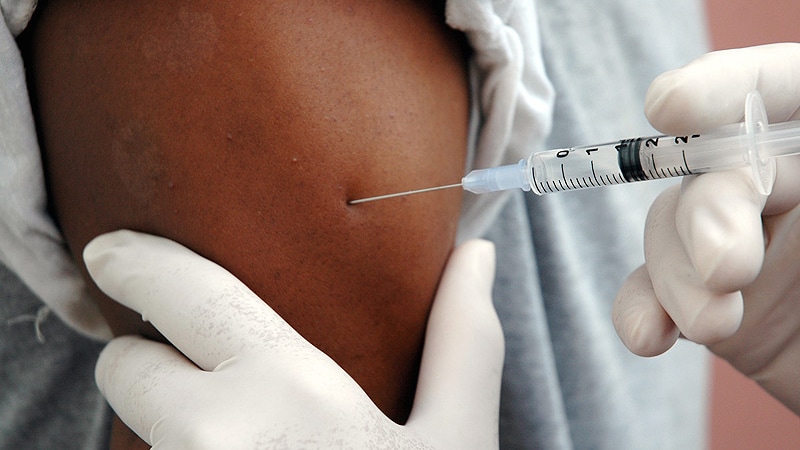
The first report on responses to COVID-19 vaccination in cancer patients suggests that for these patients, the immune response that occurs after the first dose of vaccine is reduced compared to the response that occurs in healthy individuals. health. The new findings, which are expected to be released as a pre-print, cast doubt on the UK’s current policy of delaying the second dose of the vaccine.
Delaying the second dose can leave most cancer patients completely or partially unprotected. In addition, such a delay has implications for the transmission of the virus in the vicinity of the cancer patient as well as for the evolution of variants of the virus that could be of concern, the researchers conclude.
The data comes from a UK study that included 151 cancer patients and 54 healthy controls. All participants received the COVID-19 mRNA BNT162b2 vaccine (Pfizer-BioNTech).
This vaccine requires two doses. The first participants in this study received the second dose 21 days after receiving the first dose, but national guidelines subsequently changed and the remaining participants had to wait 12 weeks to receive their second dose.
The team reports that in health controls, the immune efficiency of the first dose was very high (97% efficiency); in contrast, in patients with solid cancers, the immune efficacy of a single dose was remarkably low (39%), and it was even lower in patients with hematologic cancers (13%).
The second dose of the vaccine dramatically and rapidly increased immune effectiveness in patients with solid cancers (95% within 2 weeks of receiving the second dose), the researchers add.
Too few patients with hematologic cancer had received the second dose before the end of the study for clear conclusions to be drawn. Nonetheless, the available data suggests that 50% of hematologic cancer patients who received the booster on day 21 were seropositive at 5 weeks, compared with only 8% of those who did not receive the booster.
“Our data provide the first concrete evidence of immune efficacy following a dose of Pfizer vaccine in immunocompromised patient populations [and] clearly shows that low dose efficacy in cancer patients can be saved with an early booster on day 21 ”, commented lead author Sheeba Irshad, MD, Clinical Lecturer, King’s College London, London, UK United.
“Based on our results, we would recommend an urgent review of the vaccine strategy for clinically extremely vulnerable groups.” Until then, it is important that cancer patients continue to observe all public health measures in place, such as social distancing and protection when visiting hospitals. even after vaccination, ”added Irshad.
The article, with first author Leticia Monin-Aldama, PhD, is expected to appear on the pre-print server medRxiv. It has not been peer reviewed. The document was distributed to journalists, with comments from experts not involved in the study, by the UK Science Media Center.
These data are “of immediate importance” for cancer patients, commented
Shoba Amarnath, PhD, Research Fellow at Newcastle University, T Cell Regulation Laboratory, Newcastle University Center for Cancer, Newcastle upon Tire, UK. “These results are consistent with our understanding … We know that the immune systems of cancer patients are compromised compared to healthy controls.
“The data from the study support the idea that in patients with solid cancer, a considerable delay in the second dose will prolong the period during which cancer patients are at risk for SARS-CoV-2 infection,” she added.
Although more data is needed, “this study raises the question of whether patients with cancer, other diseases, or those undergoing therapies that affect the body’s immune response should be sped up for their second dose of the vaccine.” commented Lawrence Young, PhD, Professor of Molecular Oncology and Director of the Warwick Cancer Research Center, University of Warwick, Coventry, UK.
Stephen Evans, MSc, professor of pharmacoepidemiology at the London School of Hygiene and Tropical Medicine, stressed that the study is “primarily” observational and that “the inevitable limitations must be taken into account.
“Nonetheless, these results suggest that vaccines may not protect cancer patients as well as those who do not.” He noted that it is “important for this population to continue to observe all measures associated with COVID-19, such as social distancing and protection when visiting hospitals, even after vaccination.”
Study details
Previous studies have shown that some cancer patients have prolonged responses to SARS-CoV-2 infection, with continued immune deregulation, ineffective seroconversion, and prolonged viral shedding.
However, there is little data on how these patients respond to COVID-19 vaccination. The authors point out that among the 18,860 individuals who received the Pfizer vaccine during its developmental trials, “none with an active oncologic diagnosis was included.”
To investigate this problem, they initiated the Sars-CoV-2 Study for Cancer Patients (SOAP-02).
The 151 cancer patients who participated in this study were mostly elderly, the authors note (75% were over 65; median age was 73). The majority (63%) had solid malignant tumors; of these, 8% had advanced disease and had been living with their cancer for more than 24 months.
Healthy controls were vaccine-eligible primary health care workers who did not match the age of cancer patients.
All participants received the first dose of vaccine; 31 (of 151) cancer patients and 16 (of 54) healthy controls received the second dose on day 21.
The remaining participants were to receive their second dose 12 weeks later (after the end of the study), according to changes in national guidelines.
The team reports that around 21 days after receiving the first dose of the vaccine, the vaccine’s immune effectiveness was estimated to be 97% in health controls, compared with 39% for patients with solid tumors and only 13. % for those with hematological cancers (P <.0001 for both).
T cell responses, as assessed by the production of interferon-gamma and / or interleukin-2, were observed in 82% of healthy controls, 71% of patients with solid tumors, and 50% of those with hematological cancers.
The vaccine booster on day 21 resulted in 100% immune efficacy for healthy controls and 95% for patients with solid cancers. In contrast, only 43% of those who did not receive the second dose were HIV positive 2 weeks later.
Further analysis suggested that participants who did not have a serologic response were “evenly distributed” among the different types of cancer, but that reduced responses were more common in patients who received the vaccine within 15 days. cancer treatment, especially chemotherapy, and had undergone treatment.
The SOAP study is sponsored by King’s College London (KCL) and Guy’s and St. Thomas Trust Foundation NHS Trust. It is funded by grants from KCL Charity, Cancer Research UK and program grants from Breast Cancer Now. Investigators did not reveal any relevant financial relationship.
To learn more about Medscape Oncology, join us on Twitter and Facebook.
[ad_2]
Source link