
[ad_1]
Health workers have said “it’s a marathon, not a sprint” as new coronavirus patients “come every two minutes.”
COVID-19 hospital admissions may have declined slightly this week, but take a look at the emergency department at Barnet Hospital for a reality check.
You will see that we are still in the midst of a crisis.
Housekeeper Larisa Atanasova, famous in the hospital for her machine efficiency, can barely wipe the berries quickly enough.
She wipes and wipes and wipes; beds, rails, sinks and faucets.
“They come every two minutes,” she explains, before adding, “What can you do? The next patient arrives.
She’s right, two minutes after she disappears in another room, Davian Hunt arrives.
He is 52 years old, in good physical condition, but he can barely walk.
“Just a total lack of energy,” he said, lying on the bed. “I just want to sleep all the time.”
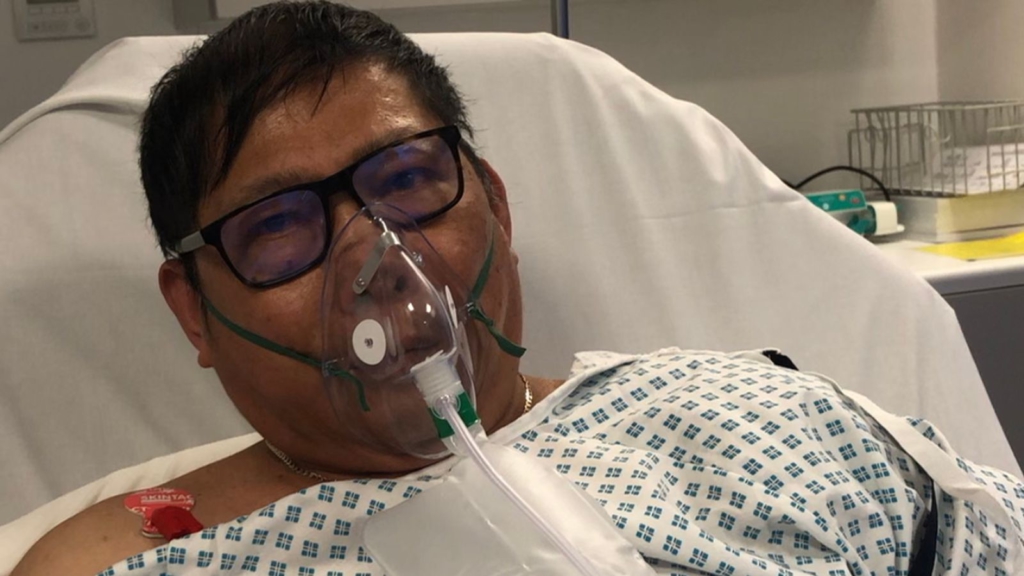
Across the department, behind a glass wall, a man, who is struggling to breathe, is about to receive a CPAP – a mouthpiece that quickly blows in oxygenated air.
63-year-old postman Felix Ramat lost his wife four days earlier to COVID-19 – now he’s dangerously ill.
In addition, her 40-year-old son-in-law is already upstairs in the ventilated hospital.
This virus tears apart families and has also spread in the A&E department.
The two nurses caring for Mr. Ramat have just recovered from the illness and are now back in the fray.
Nurse Aoibheann McCarthy says, “It has been intense. Personally, I have just returned from COVD-19. So, it was a tough struggle. I am weak. I am tired. But I’m back here. Were busy. We are full every day. We struggle, but we get through. We have good support here. About seven of us left the same week.

Upstairs in the intensive care unit from COVID-19, recovery is uncertain, but still, unconscious patients are preparing for it.
Respiratory physiotherapist Clare Bendall does what’s called telemetry – pushing the limbs back and forth, making sure the patient’s joints don’t stiffen so movement returns more easily.
She speaks to the patient through every movement while he is unresponsive on the bed.
“Now we’re going to raise that left arm. We will touch your chin. And right. Lovely, ”she said to the man attached to a fan.
She says, “Sometimes you hear our former survivors … they say they remember it as hearing accents rather than actual words.” She looks at her patient and adds, “But you know, I just think he’s a person, and I’m going to tell him what I’m doing.”
She then said to the man, “Now I’m going to stretch that knee a bit. I’m going to pull that knee towards your belly. So, we will fold this. Charming. I can’t let those knees and hips stiffen.

It is sometimes easy to forget that the people who do this kind of work absorb the horror of what is happening in the room day after day.
“I think it sounds silly, but the worst part is when we do our ward books in the morning,” Clare says. “It’s when the number of RIPs is greater than those who have reached the neighborhoods. And I think that’s where it really starts.
The emotion begins to rise behind his watched eyes.
“And they’re a lot younger – in the first wave, sorry, I remember thinking it might be mom.” It could be my aunt. And now I think it could be me. It could be my brother, my boyfriend.
“We have lost people in their thirties, in their forties. It’s heartbreaking.
Having told me that, she barely stops before pulling herself together and getting straight back to work.
No wonder a study from King’s College London last month found that nearly half of the intensive care staff surveyed over the summer reported symptoms of post-traumatic stress disorder, depression or anxiety.
Doctors around the world say critical care nurses are under the most pressure, with people like Harriet Goudie working in an adapted outpatient department on the second floor of Barnet’s sister hospital, the Royal Free, in north London.
Harriet says, “Honestly, it was really, really bad for the nurses at ITU. I think, this wave especially, it was really bad. The first wave was so stressful. And I think the pressure that ITU nurses are currently under is incredible.
Harriet cared for four patients while she normally provided individual care.
She said, “These are really sick patients. So there is multi-organ support and for the nurses at ITU it is extremely difficult to manage.
“This is an outpatient service that we had to transform into an ITU service. So it is very difficult, as you can see in these bed spaces, to try to organize all the computer equipment. We try to cram it into small spaces. We’re just running out of things like takes, for example. We don’t physically have enough outlets in some areas to be able to charge all of our equipment. “
While we are in the room together, a family video calls a barely conscious patient, telling him they love him, telling him he can get better.
They have his glasses for him as soon as he can sit down and read, and they miss him and can’t wait for him to get better and come home.
“He can hear us,” said one of them. “His eyes open.”
This is the first time this has happened.
Out of sight of their video screen, he also tries to raise his hand, but it collapses.
He’s still lying. But he listens.
And as they speak, the curtains are drawn and the porters arrive.
https://www.youtube.com/watch?v=vn9A2Ojf_v0
A man in his early sixties in the opposite bed has died, he is taken to the morgue.
A body in a white bag is placed in a blue bag on a cart and rolled up.
It’s a scene made more brutal by the tender voices and sheer strength of the family, arguing with a callous man, in the next cabin.
But they are right to hope because the patients are coming back.
Upstairs in another intensive care unit, Dima Hooper, 53, sits in her chair.
She is an NHS caterer for patient wards.
The week before, I had seen her in a state similar to the man listening to the video call.
Now, however, she has a tube down her neck and is smiling.
She gives me and my cameraman a thumbs up and indicates that in two days she hopes to be able to speak.
Just down the hall, Nicolae Ursachi, who has spent 40 days on a ventilator, is standing with the help of a walking machine and three staff.
He is out of breath in less than four steps and has to sit up. He’s also fiercely determined, and after a little rest he wants more.
Therapy assistant Chloe Davis says, “It’s like a marathon, you have to train for it. This is what we explain to patients. It’s a marathon, not a sprint. “
The same could be said of the work done by doctors – like Nicolae, their progress is slow and exhausting but driven by hope.
Source link