[ad_1]

According to a new study, it has now been proven that an antidiabetic medication commonly used to control blood sugar reduces the risk of kidney failure.
Diabetes is one of the leading causes of kidney failure. Sure with diabetes has a form of kidney disease.
The new study tested the drug canagliflozin, sold under the brand name Invokana, to determine if it could reduce the risk of kidney disease if used in combination with standard treatments.
Experts welcome the drug and other drugs that target the complications of diabetes, but warn that high costs may limit expanded access to these drugs.
The study involved 4,401 people aged at least 30 years with type 2 diabetes and chronic renal failure. The researchers randomly badigned people to take either canagliflozin or inactive placebo.
People were treated on average for two and a half years. The study was stopped early when the results showed that the drug was helping.
Compared to people taking the placebo, drug patients had a 34% lower risk of end-stage renal disease, worsening renal function or death as a result of kidney problems.
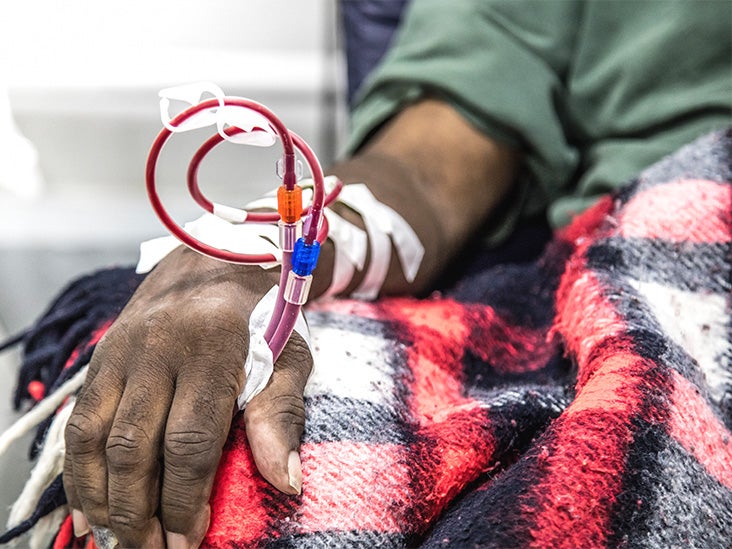
End-stage renal failure included a need for dialysis or transplantation, or signs of kidney failure.
People taking this medication also exhibited a lower risk of cardiovascular death, heart attack, stroke and hospitalization due to heart failure, compared to the placebo group.
The drug also had security issues.
An earlier study on canagliflozin revealed an increased risk of amputation of the legs, feet or toes in people who were taking the drug.
The new study found that this risk – along with the risk of bone fractures – was similar for treatment groups and the placebo group.
However, the risk of diabetic ketoacidosis was higher in people who took the drug than in those who took the placebo. This potentially life-threatening problem occurs in people with diabetes when the body breaks down fat too quickly, making the blood acidic.
The study did not include people with advanced renal failure or people with kidney failure due to conditions other than type 2 diabetes. Further research will be needed to determine if the drug can reduce the risk of kidney disease in these groups.
The findings were published April 14 in the New England Journal of Medicine.
The study was funded by the drug's manufacturer, Janssen, a division of Johnson & Johnson. Most authors of the document work for or consult for the company.
Over the last two decades, the treatment of diabetes has evolved and is no longer limited to controlling blood glucose with insulin injections, diet and exercise.
"Preventing or delaying the progression of complications and maintaining quality of life are goals of diabetes treatment," said Dr. Lorena Wright, endocrinologist at UW Medicine in Seattle, who did not participate at the study. "It requires glycemic control but also a reduction in renal and cardiovascular risk."
Drugs such as canagliflozin are part of this new therapeutic approach. It is an SGLT2 inhibitor, which lowers blood glucose by increasing the amount of glucose that the kidneys remove in the urine.
Wright said the study confirms growing evidence that SGLT2 inhibitors have protective effects on the kidneys.
Other doctors accept the drugs to treat the complications of diabetes.
"It's extremely helpful to have a drug option that not only preserves but also improves kidney function," said Dr. Minisha Sood, Endocrinologist at Lenox Hill Hospital in New York, who did not participate in the new study. .
Dr. Theodore Strange, Associate Chair of Medicine at Staten Island University Hospital in Staten Island, NY, noted that canagliflozin may reduce the number of diabetics requiring dialysis.
However, he said that a continuous follow-up of this drug and similar drugs will be necessary to ensure the sustainability of their benefits.
"I am always optimistic with caution with this kind of results," said Strange, who did not participate in the study.
Wright added that, unfortunately, access to new drugs to treat diabetes complications is largely limited by costs.
In the United States, Invokana costs between $ 500 and $ 600 a month, with no cheaper generic version.
The costs borne by the patients vary according to their insurance. Some diets, however, may not even cover this medication.
Caremark, who is responsible for the pharmaceutical benefits of many insurance plans, recently removed Invokana from its list of drugs. This means that people on these plans who want to use this drug may pay a heavy price.
People with diabetes already have high medical expenses, spending about $ 16,750 a year on medical expenses, according to a recent study, of which $ 9,600 is directly related to diabetes.
On top of that, they had to deal with soaring prices and for insulin.
Uninsured people are the hardest hit by the cost of drugs. But even patients with insurance may not be able to pay the copays for insulin and the medications they take for diabetes and its complications.
As a result, "patients can skip drugs or simply not be able to buy them," said Wright.
Sood said he hoped "more meaningful data, such as this new study, will improve the insurance coverage of this drug and similar drugs".
Better coverage of medications to treat diabetes complications may help reduce the cost of diabetes-related kidney disease. In 2011, this almost reached , just among Medicare enrollees.
"The coverage of these drugs will reduce costly complications, such as dialysis and hospitalizations," Wright said, "and will lower morbidity and mortality rates."
Source link