[ad_1]
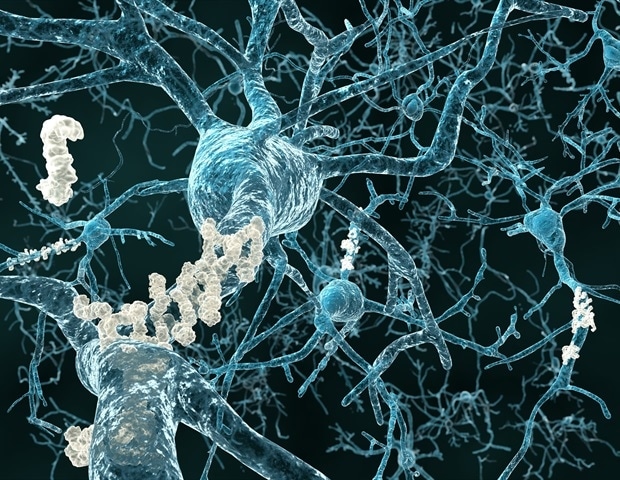
For years, research aimed at identifying the underlying cause of Alzheimer’s disease has focused on the formation of dental plaque in the brains of patients with AD. But treatments aimed at breaking up this buildup have been ineffective in restoring cognitive function, suggesting that the buildup may be a side effect of AD and not the cause itself.
New study led by a team of researchers at Brigham Young University finds new support at the cellular level for an alternative theory that is gaining strength: Alzheimer’s disease could actually be the result of metabolic dysfunction in the brain . In other words, it is increasingly clear that diet and lifestyle are at the heart of Alzheimer’s disease.
Alzheimer’s disease is increasingly referred to as brain insulin resistance or type 3 diabetes. Our research shows that there is likely a lifestyle origin for the disease, at least to some extent. “
Benjamin Bikman, senior study author and professor, physiology and developmental biology, Brigham Young University
For the new study, published in an academic journal Alzheimer’s and dementia, the BYU research team examined the RNA sequences in 240 postmortem brains affected by Alzheimer’s disease. They were specifically looking at the gene expression of supporting cells in the nervous system during two types of metabolism: glucose metabolism, where carbohydrates are broken down for energy, and what’s called ketolytic metabolism.
Ketolytic metabolism involves the brain making energy from ketones, molecules made in our bodies when the hormone insulin is low and we burn relatively higher amounts of fat. The popular “keto diet” gets its name from the process, as this low-carb, high-protein diet lowers insulin levels and causes the body to burn fat instead of carbs and produce ketones.
The researchers found a generalized alteration in glucose metabolism in these nervous system support cells of the brains of former patients with Alzheimer’s disease, but a limited alteration in ketolytic metabolism.
The finding is significant because the brain is like a hybrid engine, with the ability to get fuel from glucose or ketones, but in the Alzheimer’s brains studied there appears to be a fundamental genetic deficit in the brain’s ability to use glucose.
“We turned our brain’s hybrid engine into a single-fuel system that just doesn’t work,” Bikman said. “And so the brain, which is gradually becoming deficient in its ability to use glucose, is now calling for help; he is starving in the midst of plenty. The body is swimming in a sea of glucose, but the brain simply can’t use it.
“The inability to utilize glucose increases the value of ketones. However, because the average person eats insulin-spiked foods so frequently, there are never any ketones available to the brain,” Bikman added. “I see these results as a problem that we have created and that we are making worse.”
Previous research has observed that the brains of people with AD have a quantifiable reduction in the ability to absorb and use glucose, but this article is the first to show that this actually occurs at the cellular level. It is a significant contribution to the growing paradigm shift with regard to the scientific view of the causes of Alzheimer’s disease.
And because ketolytic metabolism appears to continue to work well in people with AD, even when glucose metabolism gives way, the article concludes that treatments involving ketones may be able to support brain metabolism and slow associated cognitive decline. to disease.
Source:
Journal reference:
Saito, ER, et al. (2021) Alzheimer’s disease alters the expression of glycolytic and ketolytic oligodendrocytic genes. Alzheimer’s and dementia. doi.org/10.1002/alz.12310.
Source link