[ad_1]
(MENAFN – The Conversation) The best defense against Ebola outbreaks is early detection. If detected early enough, an outbreak can be prevented through targeted, low-tech interventions such as isolation of infected people and their contacts. But our research suggests that most early detection and intervention opportunities are missed. In fact, we estimate that most of the time, when the Ebola virus pbades from one wildlife to another, it is not detected at all.
Every outbreak of Ebola begins with an "overflow event", in which a person is infected with an animal – a bat for example. From there, people can infect others and quickly, an epidemic can become uncontrollable. Once the epidemic has spread to many places, it is extremely difficult to control it, as has been shown by the outbreaks of recent years.
An essential feature of Ebola virus infections is that a few first cases infect many other people, but that most cases (about 65%) do not infect anyone else. This means that any isolated case – such as the first case of Ebola overflow – is probably the only case. The discovery of these cases is as important as the early detection of an outbreak, as it is impossible to predict which overflow events will turn into complete outbreaks. But since the Ebola virus was first detected in 1976, only eight groups of five cases or fewer were detected, compared with 26 groups of at least six cases.
Only two single-case contagion events have already been detected (with the exception of accidental laboratory infections), but we expect that it will be the largest cluster size common. The most plausible reason for this unexpected situation is that many small clusters of Ebola have occurred without anyone realizing it.

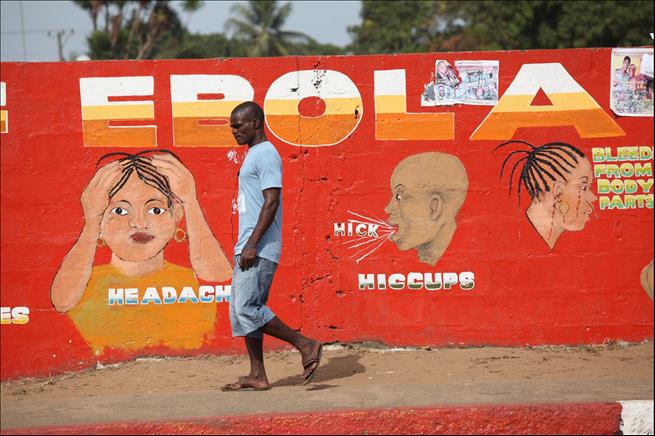
The dogfish can transmit the Ebola virus to humans.
Jeffrey Paul Wade / Shutterstock
Computer simulation
To find out how many of these small clusters occurred, we simulated thousands of Ebola outbreaks based on published data from previous outbreaks. From these simulations, we have determined the frequency with which we expect an overflow event to disappear rapidly relative to the frequency with which we expect it to become a true outbreak. This allowed us to compare the size of the epidemics we expect to see with those reported. We used these comparisons to estimate the detection rates of clusters of different sizes. Among different sets of hypotheses, we estimated that less than half of the clusters of Ebola and less than 10% of isolated cases were detected.
This result suggests that we are completely missing many cases. Since we estimate particularly low detection rates for small clusters, this also suggests that we rarely detect outbreaks in their infancy.
We rarely find outbreaks of Ebola while they are still easy to manage. The main reasons are surprisingly simple. Ebola is much rarer than other types of severe fever in areas of sub-Saharan Africa where it tends to occur. Countries in this region have some of the lowest primary health care infrastructure in the world, making them poorly equipped to detect a rare cause of fever among all common causes.
Many primary health care facilities do not have sufficient resources to test even the most common causes of fever, not to mention Ebola. Without accurate diagnosis, they must rely on symptom-based detection. But the Ebola virus is so rare that a single case of severe fever, even in case of bleeding, is more likely to be caused by malaria, typhoid or yellow fever. Most doctors and public health workers in many areas have never seen a single case of Ebola. Therefore, the mere detection of Ebola is not reliable.
Investment in primary health care
It is probably impossible to reliably detect outbreaks in the first cases based solely on symptoms. To detect and combat epidemics early, we need to invest in primary health care and public health capacity.
It is at this local level, mainly in clinics and hospitals, that potential outbreaks are reported for the first time. It is also at this level, mainly through district health management teams, that measures such as quarantine can be introduced quickly enough to control an early epidemic.
This capacity is not only important for Ebola, as improving the capacity of local health workers to diagnose and treat disease quickly can improve outcomes. A more accurate diagnosis of bacterial infections compared to viral infections, for example, can help combat increasing resistance to drugs.
Although important, international responses to outbreaks are often slow, complicated and costly. The case of Ebola shows how these types of responses are also not suitable for intervening at the most crucial moments. Instead, it is time for us to invest more in the kind of local primary capacity that can detect and limit outbreaks at the source.
Ebola
MENAFN1506201901990000ID1098639657
[ad_2]
Source link