[ad_1]
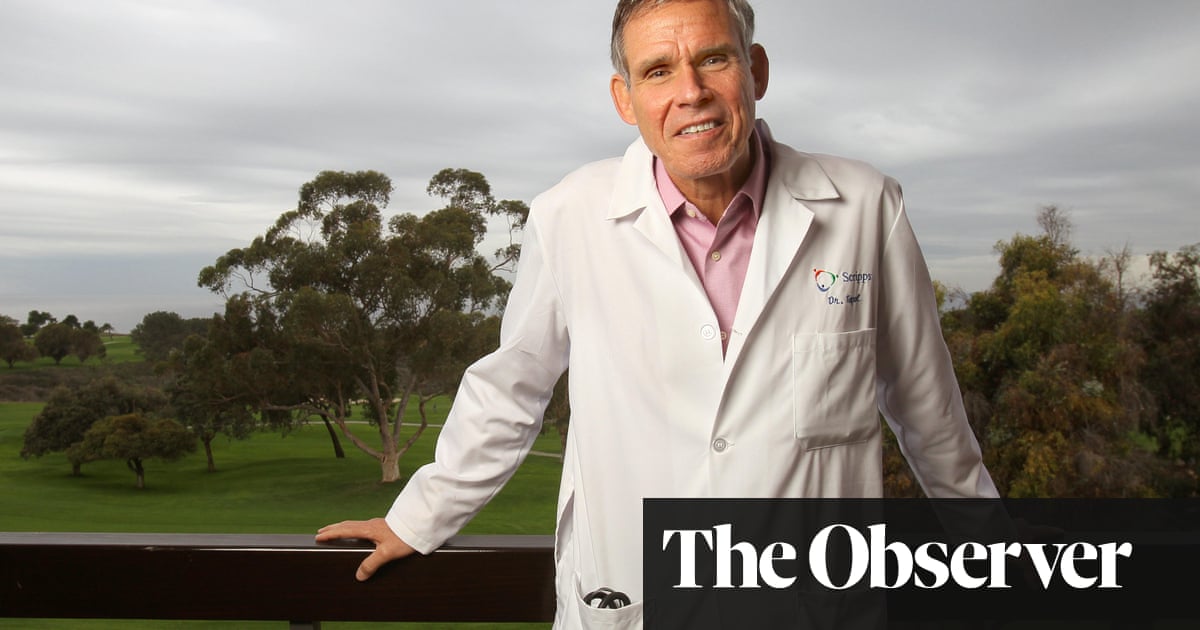
Eric Topol is a cardiologist and an American geneticist. Among his many roles, he is founder and director of the Scripps Research Translational Institute in California. Previously, he published two books on the potential of Big Data technologies to transform medicine, with his third, Deep medicine, look at the role that artificial intelligence could play. He has served on the advisory boards of many health sector companies. Last year, he published a report on the need for the NHS to change to adopt digital advances.
Your field is cardiology – what motivates you as a doctor?
Well, the patients. But also the wider mission. Yesterday, I spent the whole day at the clinic – I love seeing patients – but I also try to use every possible resource to think about how we can do things better, how can we improve the links, accuracy and precision of our care.
What is the most promising medical application in artificial intelligence?
In the short term, taking pictures and getting much better accuracy and speed – not that it would supplant a doctor, but rather it would be a first pbad, a first screening supervised by a doctor. So, whether it's a medical scanner, a pathology slide, a skin lesion or a colon polyp, that's the short-term story.
You talk about a future where monitoring settings are constantly being monitored – How is this promising?
You are ahead of the curve in the UK. If you think you have a urinary tract infection, you can go to the pharmacy, get an AI kit that accurately diagnoses your urinary tract infection and get an antibiotic – without having to see a doctor. You can get an Apple Watch that will detect your heart rate and, if there is a problem, send you an alert to take your cardiogram.
Is there a danger that it will mean are more and more people part of the "troubled well"?
It's even worse now because people are doing a search on Google, then think that they have an illness and are going to die. At least that is your data so that it has a better chance of being significant.
This is not for everyone. But even if half of people believe it, there is a major decompression of what doctors do. This is not for life-threatening business, such as a diagnosis of cancer or a new diagnosis of heart disease. This is for the most common problems – and for most of them, if people wish, the diagnosis of AI will be made without a doctor.
If you had an AI generalist, he could listen to and respond to descriptions of patients' symptoms, but would he be able to physically examine them?
I do not think you can simulate a real exam. But you can do some parts – for example, there have been recent studies of AI on coughing kids, and just by interpreting that sound by AI, you can diagnose accurately the type of lung problem that it involves.
Smart phones can be used as ultrasound imaging devices. There could be an inexpensive ultrasound probe one day. A person can image a part of his body, send this image for it to be interpreted by the AI, and then discuss it with a doctor.
One of the biggest is the eyes, the retina. You will be able to take a picture of your retina and check if your blood pressure is well controlled, if your diabetes is well under control, if you have the beginnings of diabetic retinopathy or macular degeneration – this is an exciting area for patients who Are at risk.
What are the main technical and practical barriers to the use of AI in health care?
Well, there is a long list – privacy, security, bias algorithms, inequalities – and their worsening because the AI in health care addresses only those who can afford it
You are talking about the fact that perhaps the AI could spot people who present or are at risk of developing mental health problems through the badysis of social media posts. How would it work and how would you prevent people's mental health badessment without their permission?
I was not suggesting that social media is the only window to a person's state of mind. Today, mental health can be defined objectively, whereas it was very subjective in the past. We talk about speech pattern, tone, breathing – when people sigh a lot, it denotes depression – physical activity, how people move, how much they communicate.
Facial recognition, social media postings and other vital signs such as heart rate and heart rate are then used, so that the collection of all these objective measures can be used to track the patient. A person's mood state can help show what works to get them out of this state and predict the risk of suicide.
Objective methods do better than psychologists or psychiatrists predict who is at risk. So I think that mental health and AI are promising.
Yes The AI gets a very bad diagnosis or treatment, who is sued? The author of the software or the doctor or hospital that provides it?
There is no precedent yet. When you register with an application, you waive all legal remedies. People never read the terms and conditions of course. So, the company could still be held responsible because there is no real consent. For the doctors involved, it depends on the location of this interaction. What we do know is that today there is a horrendous problem of medical errors. So if we can clean that up and make it a lot less, it will go in the right direction.
Jeremy Hunt asked you in 2018 to conduct a review of how the NHS workforce will need to change "to provide a digital future". What is the biggest change you recommended?
I think the biggest change has been to try to accelerate the integration of AI to give the time it took, to restore the patient – doctor relationship, to which we all participated in 30 or 40 years ago. There is a new unprecedented opportunity to seize this and restore the health care that has been largely lost.
In the USA, different Democratic candidates for 2020 suggest a government supported system – a little like our NHS. Does this enable the AI in care to flourish without insurers discriminate against patients with "wrong data"and allow the AI to fulfill his promise?
Well, I think that certainly helps. If you have a single system where you implement AI and you have all the data in a common source, it is much more likely to succeed. The effectiveness of the NHS in providing care with better results than the United States at a lower cost per person is a lot because you have a superior model.
• Eric Topol's Deep Medicine is published by Basic Books (£ 25). To order a copy for £ 22, go to guardianbookshop.com. UK free p & p on all online orders over £ 15
Source link