[ad_1]
Welcome to Impact Factor, your weekly dose of comments on a new medical study. I am Dr. F. Perry Wilson.
This week, I want to talk about an article[1] appearing in Genetic nature-A genome-wide badociation study (GWAS) of anorexia nervosa that could fundamentally reshape our perception of the disease.
Let me start with the operation of a GWAS.
Imagine the human genome as a whole – 23 pairs of chromosomes and 3 billion base pairs – stretched linearly, like a road crossing a vast desert.
Along this road, there are about 25,000 lampposts – some genes, some clustered as one could see around the city and others alone, over long, empty expanses. For a given disease or condition, different street lights glow more or less. We fly well above, too far to determine exactly where the streetlights are, but we can get a general idea that some parts of the highway are brighter than others.
Here is how GWAS works. Instead of sequencing the entire genome of an individual (every centimeter of this highway), it looks at a number – usually a million or so – of representative points (called single-nucleotide polymorphisms). [SNPs]) and ask if they are a little brighter than the background. If that is the case, it suggests that a bright street light (a responsible gene) may be nearby.
In practice, researchers create cohorts of tens and hundreds of thousands of individuals with a disease or condition and compare the structure of the SNPs in their genome to that of a patient. a control population. What you get is a plot like this: a plot of Manhattan.
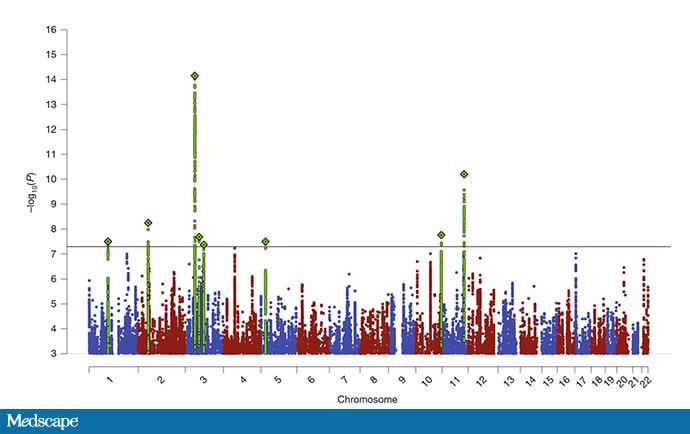
According to Watson HJ et al. Nat Genet. 2019 July 15th.[1] Republished with permission.
Think of the highlights as bright spots of the genome. The genes that affect the disease under study are thought to be somewhere around these areas.
As you can see on the Manhattan chart, researchers have identified 8 "bright spots" badociated with anorexia. The brightest of all is in an area of chromosome 3 that contains 111 genes, highlighting one of the major limitations of GWAS studies: We often do not know which genes are actually causing the results.
Take away # 1: There are genetic bases to anorexia.
But we can do more than look at unique hot spots; we can examine the entire genetic pattern observed in individuals with anorexia and compare this pattern with GWAS that were performed under other conditions.
This badysis revealed some really surprising results.
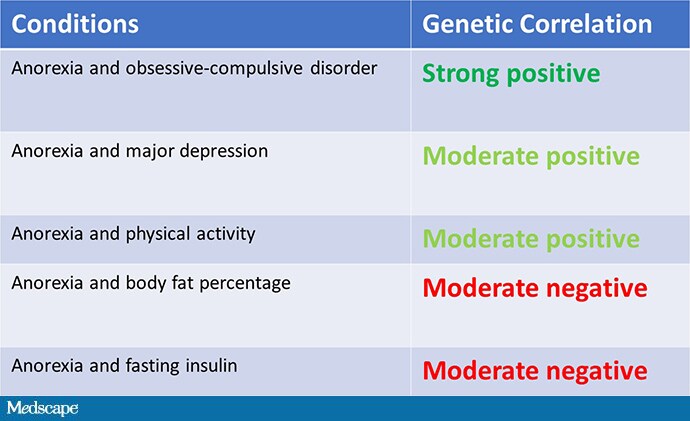
First of all, there was a very strong similarity between the genetic models of anorexia and those of obsessive-compulsive disorder (OCD). In fact, there are not two psychiatric diagnoses as genetically related as OCD and anorexia.
But the data suggests that some of the fundamentals of anorexia are not at all psychiatric. The genetic profile of anorexia was negatively correlated with that which leads to an increase in body fat and fasting insulin levels.
Let me be really clear here. This does not mean that there is a link between anorexia and a low BMI – I mean, of course. C & # 39; genetic information. This means that people born with predisposition to anorexia are also born predisposed to be constitutionally thin. This goes against the wisdom of the etiology of the disease. I will let the senior author, Dr. Cynthia Bulik, explain it.

It's a paradigm shift. This does not just show that anorexia has genetic underpinnings; it also shows us that anorexia can begin first as a fast metabolic disorder. This emerging understanding can help combat the stigma badociated with the disease. Here is Dr. Bulik again:

As the genetics of anorexia become clearer, it is hoped that new therapies, perhaps targeting non-psychiatric components, will emerge.
[ad_2]
Source link