[ad_1]
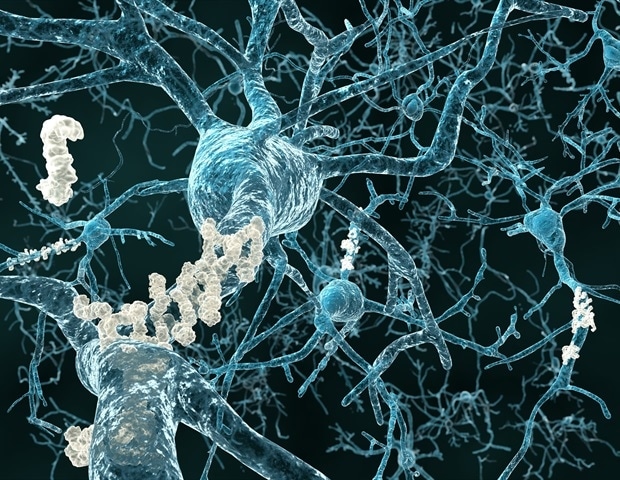
In the first study using whole genome sequencing (WGS) to uncover rare genomic variants associated with Alzheimer’s disease (AD), researchers identified 13 of these variants (or mutations). In another new finding, this study establishes new genetic links between AD and the function of synapses, which are the junctions that transmit information between neurons, and neuroplasticity, or the ability of neurons to reorganize the brain’s neural network. . These findings could help guide the development of new therapies for this devastating neurological disease.
Researchers at Massachusetts General Hospital (MGH), Harvard TH Chan School of Public Health, and Beth Israel Deaconess Medical Center report these findings in Alzheimer’s and dementia: the journal of the Alzheimer’s Association.
Over the past four decades, the MGH has pioneered research into the genetic origins of AD, led by Rudolph Tanzi, PhD, Vice President of Neurology and Director of the Genetics and Research Unit. aging hospital. Notably, Tanzi and his colleagues co-discovered genes that cause the early onset (before age 60) of familial AD (i.e. a form that runs in families), including the precursor of amyloid protein (A4) (APP) and the presenilin genes (PSEN1 and PSEN2). Mutations in these genes cause amyloid plaques to build up in the brain, a hallmark of AD.
The following 30 AD gene variants that have been discovered are primarily linked to chronic inflammation of the brain (or neuroinflammation), which also increases the risk of this dementia. However, the loss of synapses is the neurological change that most closely correlates with the severity of dementia in Alzheimer’s disease, but no clear genetic link between the disease and these vital connections had been identified previously. “It has always been quite surprising that whole genome screens have failed to identify Alzheimer genes that are directly involved in synapses and neuroplasticity,” says Tanzi.
Prior to this article, the genome-wide association study (GWAS) was the primary tool used to identify genes for AD. In a GWAS, the genomes of many individuals are scanned for common genetic variants that occur more frequently in people with a given disease, such as AD. But to date, the common genetic variants associated with Alzheimer’s disease have accounted for less than half of the heritability of AD. A standard GWAS misses the rare gene variants (those that occur in less than 1% of the population), a problem solved by the WGS, which scans every bit of DNA in a genome.
This article takes us to the next step in discovering the disease gene by allowing us to examine the entire sequence of the human genome and assess rare genomic variants, which we could not do before. “
Dmitry Prokopenko, PhD, McCance Center for Brain Health, MGH, lead author of the study
Identifying less common genetic mutations that increase the risk of AD is important because they may contain critical information about the biology of the disease, Tanzi says. “Rare gene variants are the dark matter of the human genome,” he says, and there are many: of the three billion nucleotide base pairs that make up a complete set of DNA, each person has 50 to 60 millions of gene variants. -and 77% are rare.
In their quest to find rare variants of the AD gene, Tanzi, Prokopenko, and their colleagues performed WGS analyzes on the genomes of 2,247 people from 605 families including multiple members diagnosed with AD. They also analyzed WGS data sets of 1,669 unrelated individuals. The study identified 13 previously unknown rare gene variants associated with AD. Strikingly, these genetic variants were associated with synapse function, neural development, and neuroplasticity.
“With this study, we believe we have created a new model to go beyond the standard GWAS and the association of disease with common genomic variants, in which you miss a large part of the genetic landscape of the disease,” says Tanzi, who sees the potential of their methods to be used to study the genetics of many other conditions. Additionally, he plans to use “Alzheimer’s in a dish” – three-dimensional cell culture models and brain organoids that he and his colleagues have developed over the past decade – to explore what happens when mutations rare identified by this article are inserted into neurons. . “It could guide us in the discovery of new drugs,” says Tanzi.
Source:
Massachusetts General Hospital
Source link