[ad_1]
The COVID-19 pandemic is caused by a beta coronavirus called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). This coronavirus causes acute respiratory syndrome which was first identified in Wuhan, China in December 2019. This new zoonotic virus has put the world on high alert, quickly becoming a pandemic.
Clinically, COVID-19 (2019 coronavirus disease) is a heterogeneous disease. The characteristics range from cough, sore throat, fever, myalgia or arthralgia, fatigue, headache, gastrointestinal problems, loss of smell or taste, between other symptoms less numerous.
Identifying risk factors is essential for rapid diagnosis, better monitoring and prognosis of infected patients. Age and co-morbidities (such as diabetes, hypertension, stroke, cancer, kidney disease, and high cholesterol) have been shown to be risk factors associated with mortality in COVID-disease. 19.
New analysis of lab results from COVID-19 patients reveals a strong association of risk with hematologic values such as leukocytes and neutrophils.
To quickly discriminate between patients with severe and non-severe COVID-19, researchers in Peru looked for prognostic signatures in blood samples from COVID-19 patients. Virgilio E. Failoc-Rojas et al. examined laboratory results and clinical prognosis of COVID-19 patients from a hospital in the Peruvian Amazon. The results of this fascinating new study are published on the pre-print server medRxiv *.
The researchers found that increased levels of leukocytes, neutrophils, low levels of lymphocytes, monocytes and eosinophils had a strong association with mortality.
“Parameters such as leukocytes and neutrophils were statistically much higher in deceased patients.”
The study
The study cohort was 127 patients hospitalized at a hospital in Ucayali (located in the central jungle, in eastern Peru). All patients received a confirmed diagnosis of COVID-19 during the period March 13 to May 9, 2020. Confirmation of COVID-19 was confirmed by polymerase-transcriptase chain reaction (RT-PCR) test nasopharyngeal swab samples and a rapid immunochromatographic test. This population has experienced a mortality of 75 people.
Laboratory evaluations included leukocytes, neutrophils, platelets, RDW-SD (distribution width of red blood cells with standard deviation), RN / L (neutrophils to lymphocyte ratio), fibrinogen, CRP (C-reactive protein) , D-dimer, DHL (Lactate dehydrogenase), hematocrit, monocytes and eosinophils.
While the study population had overall high levels of biochemical and hematological values, researchers stratified single observations based on mortality.
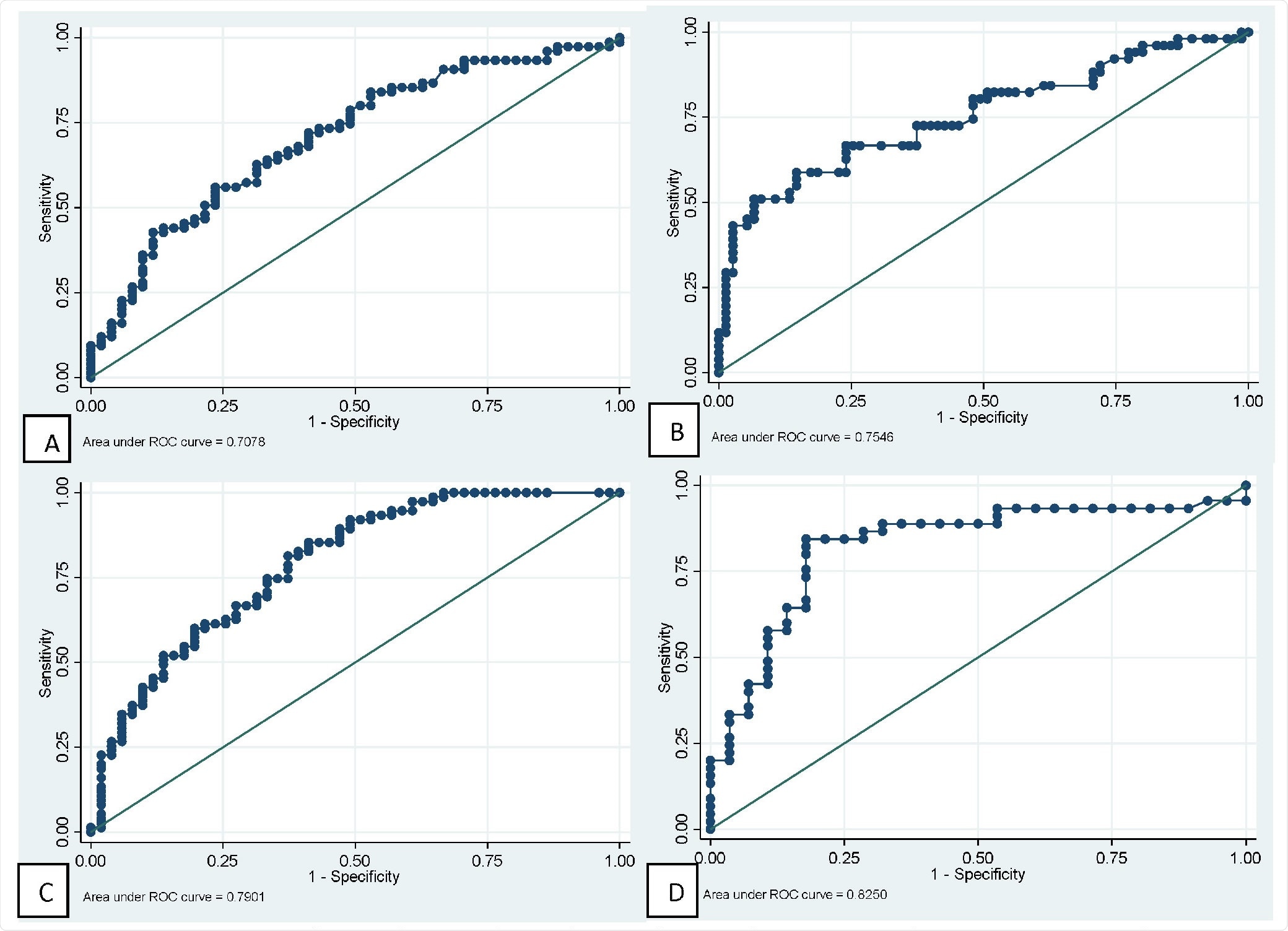
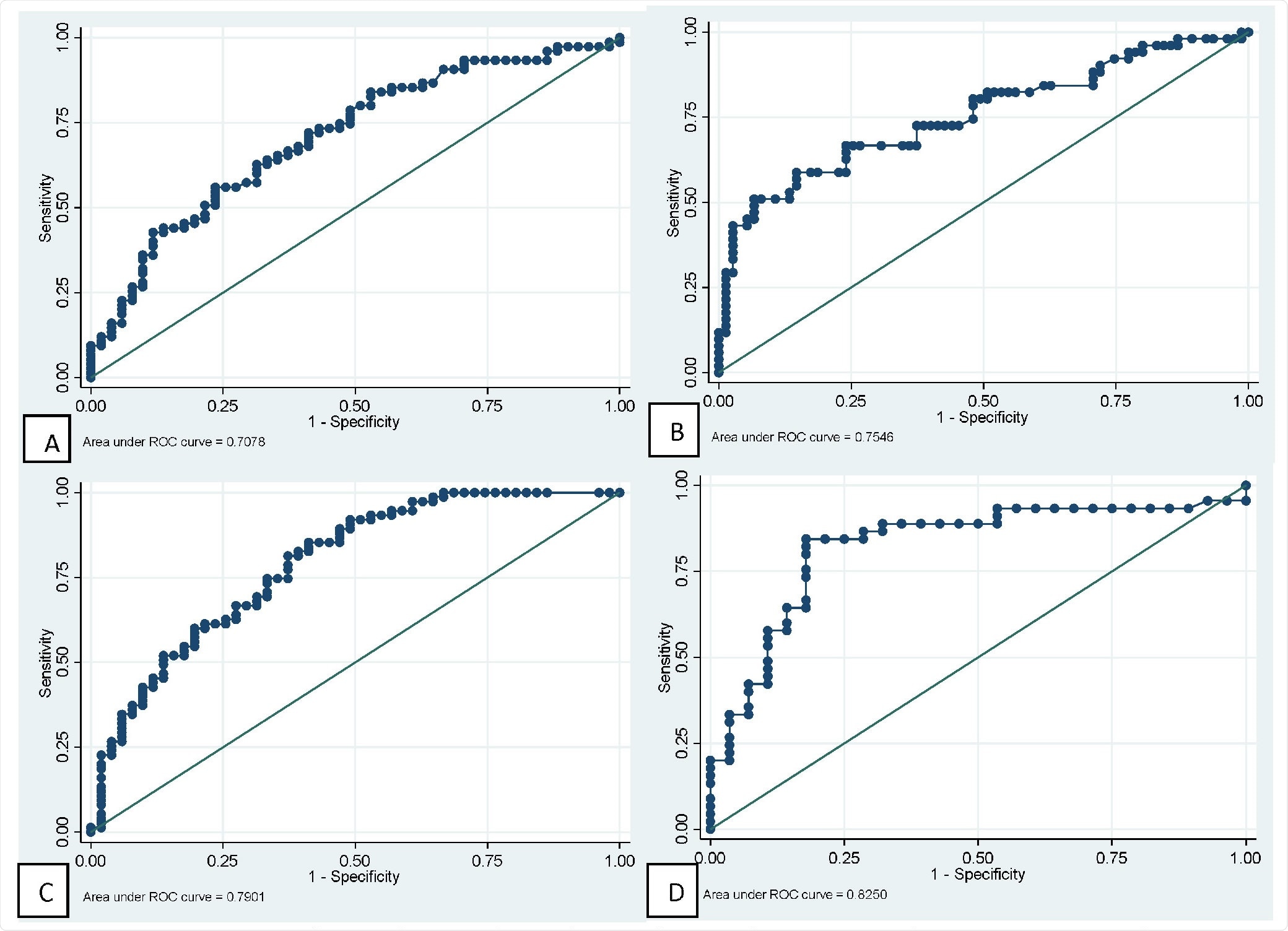
ROC curves of major hematologic tests to predict mortality in patients with COVID-19. A: Neutrophilic. B: lymphocytes. C: neutrophils / lymphocytes ratio. D: fibrinogen.
They found: 1) leukocytes and neutrophils were higher in deceased patients 2) they also had lymphocytopenia (abnormally low levels of lymphocytes) compared to normal values in survivors (720 vs 1360 respectively), and 3) low levels of monocytes and eosinophils.
The researchers also found that other parameters such as RN / L and fibrinogen were higher in the deceased population than those who survived. Similar platelet values observed, red blood cell distribution width with standard deviation (RDW-SD) and D-dimer, in both groups.
Corroborating with other studies, they observed in this study that for every one year increase in age, the probability of death increased by 4%.
IRR (Incidence Risk Ratio) analysis for numerical variables showed results strongly associated with hematological values such as leukocytes (on the 2,500 unit scale), neutrophils (on the 2,500 unit scale) ; on the contrary, it is observed that the increase of 1000 units of lymphocytes, the probability of dying decreased by 48%, write the researchers.
Notably, the researchers found the most significant association of D-dimer with death. They found that with high levels of D-dimers – for every 1 mg / L increase – the risk of dying increased by 25%. D-dimer is a degradation product of fibrin indicating hypercoagulability and thrombotic events.
Conclusion
To date, COVID-19 has claimed more than 2.26 million lives out of over 104 million confirmed COVID-19 infections worldwide. The findings from this study are important to understanding the prognosis of patients with COVID-19. This new information can help provide timely therapeutic support and offer a chance to progress patients from severe to normal.
We know that COVID-19 has a significant impact on the hematopoietic system and hemostasis; leukocytosis, lymphopenia, and thrombocytopenia are associated with increased severity and even death in COVID-19 cases. Lymphopenia can be considered prognostic.
This study examines the biochemical and hematological parameters of patients with COVID-19 in association with the risk of mortality. In this context, researchers find various parameters strongly associated with death.
These observations in COVID-19 patients – severe and not severe – will help to better understand the key features. Such a study, looking for prognostic markers for various symptomatic diseases like COVID-19, spearheads the research, control and prevention of future diseases.
*Important Notice
medRxiv publishes preliminary scientific reports which are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or treated as established information.
Journal reference:
- Prognosis and hematologic results in patients with COVID-19 in an Amazonian population of Peru, Sebastian Iglesias-Osores, Arturo Rafael-Heredia, Eric Ricardo Rojas-Tello, Washington A. Ortiz-Uribe, Walter Leveau-Bartra, Orison Armando Leveau -Bartra, Miguel Alcantara-Mimbela, Lizbeth M. Cordova-Rojas, Elmer Lopez-Lopez, Virgilio E. Failoc-Rojas, medRxiv, 2021.01.31.21250859; doi: https://doi.org/10.1101/2021.01.31.21250859, https://www.medrxiv.org/content/10.1101/2021.01.31.21250859v1
Source link