.jpg)
[ad_1]
Spanish researchers have shown that studying the hypoxia signaling pathway may offer treatment opportunities for coronavirus disease 2019 (COVID-19).
The team conducted a study showing that hypoxic (oxygen deficient) conditions reduced the expression of host cell receptors for the causative agent – severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
.jpg)
Hypoxic conditions reduced expression of angiotensin-converting enzyme 2 (ACE2) – the major host cell receptor required for viral attachment and entry. They also decreased the expression of heparan sulfate (HS), another receptor known to be necessary for the attachment of SARS-CoV-2.
The team – from the Basque Alliance for Research and Technology in Derio and the Basque Foundation for Science in Bilbao have also shown that hypoxia decreases the levels of HS by reducing the expression of the main proteoglycans containing HS ( HSPG) – syndecan-1 and syndecan-3.
“Our study indicates that hypoxia works to prevent infection with SARS-CoV-2, suggesting that the hypoxia signaling pathway may offer therapeutic opportunities for the treatment of COVID-19,” Asis writes Palazon and his colleagues.
A pre-printed version of the research paper is available on the bioRxiv * server, while the article is subject to peer review.
Hypoxia, a common feature of COVID-19
A common feature in patients with COVID-19 is moderate to severe hypoxia, but how hypoxia influences SARS-CoV-2 infectivity and disease pathogenesis is not yet clear.
However, studies have shown that low oxygen levels may reduce the infectivity of SARS-CoV-2 and the severity of the disease.
The process of infection with SARS-CoV-2 involves the receptor binding domain (RBD) in the 1 (S1) subunit of a viral surface protein called a peak. This RBD interacts with the ACE2 and HS host cell receptors before the peak 2 (S2) subunit mediates fusion between virus and cell membrane.
Research has shown that ACE2 expression is regulated by hypoxia in a time-dependent manner, and epidemiological data suggests that the severity of COVID-19 decreases in high altitude areas.
In addition, syndecans – the major HSPGs – have also been shown to be regulated differently by hypoxia.
“Our hypothesis is that hypoxia influences the cellular attachment of SARS-CoV-2 in host cells by modulating the expression of viral entry and attachment receptors on epithelial cells,” explains Palazon and the team. .
What did the researchers do?
To determine whether hypoxia affects cell binding of the spike protein, the researchers subjected human lung epithelial cells (NCI-H460) and Vero E6 cells incubated with RBD and S1 at different oxygen concentrations (21% vs. 1% oxygen).
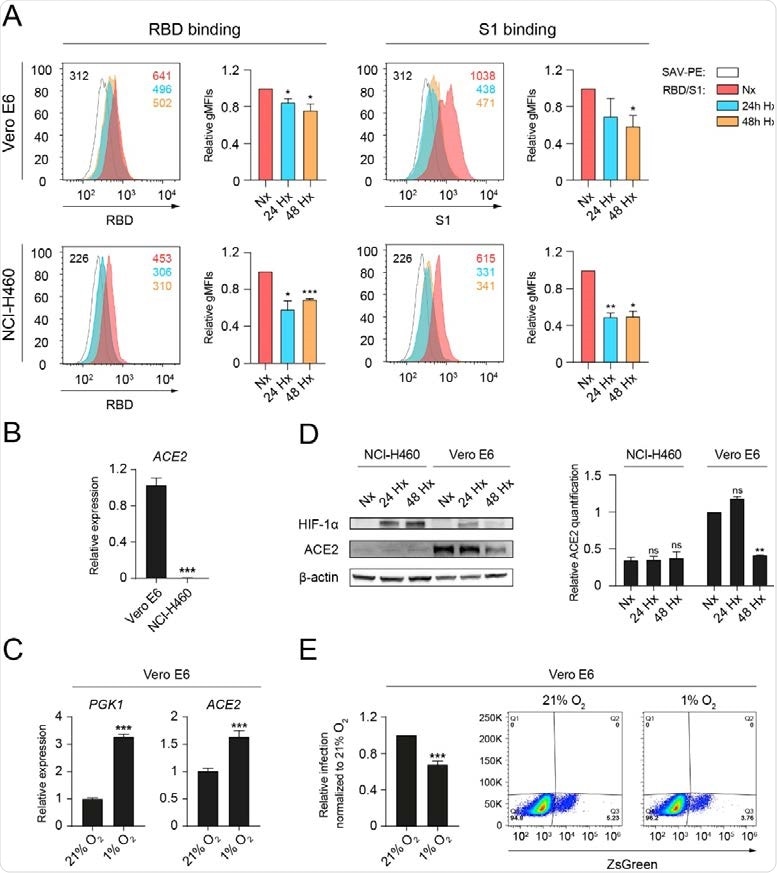
Hypoxia reduces the binding of RBD and S1 to epithelial cells and decreases levels of ACE2 protein. (A) Receptor binding domain binding (RBD) (left) or S1 subunit (S1) (right) to Vero E6 (top, n = 3, unpaired t-test) or NCI-H460 ( bottom, n = 2, unpaired t test) cells cultured under normoxia (21% oxygen) or hypoxia (1% oxygen) for 24 and 48 hours, measured by flow cytometry. A representative histogram showing the geometric mean fluorescent intensity (gMFI) value for each condition is displayed. (B) Relative expression of the ACE2 gene on Vero E6 and NCI-H460 measured by Q-PCR (n = 3, unpaired t test). (C) Relative gene expression of PGK1 (left) and ACE2 (right) on Vero E6 cells cultured under normoxia or hypoxia for 24 hours (n = 3, unpaired t test). (D) (left) Western blot of HIF-1α, ACE2 and β-actin on Vero E6 and NCI95 H460 cells cultured under normoxia or hypoxia for the indicated time points. (Right) Relative quantification of ACE2 protein expression by densitometry (n = 2, 2-way ANOVA). (E) Relative infection of Vero E6 cells with pseudotyped viral particles expressing SARS98 CoV-2 spike protein, measured by flow cytometry based on ZsGreen expression (n = 4 independent experiments). Error bars represent SEM. The asterisks represent the p values (*, ≤ 0.05; **, <0.01; ***, <0.001).
Under hypoxic conditions (1% oxygen), the binding of RBD and S1 was significantly reduced in both cell lines.
The team evaluated the expression of the ACE2 gene using quantitative PCR (polymerase chain reaction) to explore the mechanism underlying this reduced binding.
This revealed that only Vero E6 cells exhibited detectable levels of ACE2. While hypoxia significantly increased ACE2 transcription in Vero E6 cells, it significantly reduced total ACE2 protein levels.
The researchers say this could at least partially explain the reduced cellular binding of RBD and S1.
They showed that Vero E6 cells cultured under hypoxic conditions exhibited a decreased rate of infection with pseudotyped SARS-CoV-2 lentiviral particles.
“The observed reduction in ACE2 protein levels contrasts with the early transcriptional increase in this gene,” the team explains.
However, this likely results from the binding of hypoxia-inducible factor (HIF) transcription factors to hypoxia response elements on the ACE2 promoter, they add.
“The observed difference between RNA and ACE2 protein levels could be explained by protein degradation, cleavage or time adaptation to hypoxia.”
What about the NCI-H460 cell line?
The NCI-H460 cell line contains significantly fewer ACE2 transcripts compared to Vero E6 cells and does not express detectable levels of ACE2 protein.
However, the interaction of RBD and S1 with these cells was still strongly inhibited by hypoxia, indicating the presence of additional SARS-CoV-2 binding factors that are regulated by hypoxia.
Next, the team explored whether the host cell’s HS receptor levels were altered under hypoxic conditions.
This revealed that the total level of HS expressed on NCI-H460 and Vero E6 cells was significantly decreased under hypoxic conditions.
The researchers then used flow cytometry to assess syndecan expression and found that syndecan-1 and syndecan-3 were the most abundant of the two cell lines.
The study found that hypoxia downregulated syndecan-1 levels on NCI-H460 cells and syndecan-3 levels on Vero E6 cells.
Palazon and colleagues say the study shows that hypoxia reduces SARS-CoV-2 binding of host cells by at least two different mechanisms: hypoxia lowers levels of the viral ACE2 entry receptor and levels of HS. in cell surface HSPGs.
“The significance of these findings to pathophysiological oxygen levels remains unexplored,” the researchers write.
“In this context, elucidating the role of the HIF signaling pathway could unlock new therapeutic targets which, when modulated, reduce the initial virus-host interaction and viral load,” they conclude.
*Important Notice
bioRxiv publishes preliminary scientific reports which are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or treated as established information.
Source link