[ad_1]

January 18, 2019 – 16:14 AMT
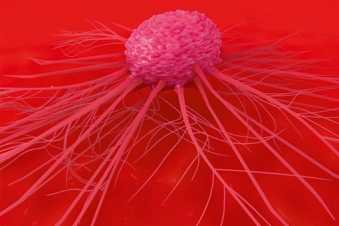
PanARMENIAN.Net – Results of the largest study of Hepatitis B and C and HIV The prevalence of infection in cancer patients shows an alarming rate of both undiagnosed acute and chronic hepatitis B and C. Hepatitis B and C are serious but treatable viral infections that cancer patients should be aware of, as they can cause life-threatening complications when certain cancers treatments are used.
Researchers at the SWOG Cancer Research Network, an international group of cancer clinical trials funded by the National Cancer Institute (NCI), part of the National Institutes of Health, conducted the study , whose results appear today in JAMA Oncology. The SWOG team found that a significant portion of newly diagnosed cancer patients with hepatitis B or C were unaware of their viral infection. Many had no identifiable risk factors for these infections, such as injecting drug use.
The findings suggest that universal screening for hepatitis B or C could be warranted in community-based cancer clinics, which would allow physicians to help patients avoid liver failure, kidney disease, or kidney disease. 39, other complications of hepatitis. Universal testing would also help care teams make more informed choices about cancer treatment, including avoiding those that could trigger the reactivation and spread of the hepatitis virus, thereby making cancer patients even more sick. There is some evidence that anti-CD20 treatments, such as rituximab, as well as hematopoietic cell transplantation, treatments for lymphoma and leukemia, can trigger the reactivation and multiplication of some infectious viruses.
"As a patient or cancer doctor, I would like to know the results of a hepatitis test," said Scott Ramsey, MD, Ph.D., SWOG researcher and director. of the Hutchinson Institute for Cancer Research (HICOR). ) at the Fred Hutchinson Cancer Research Center. "The presence of a life-threatening infection could be a very important driver of care, and in medicine more knowledge is always better."
The SWOG study, known as S1204, is distinguished by its large size and its sample of diverse patients.
Between 2013 and 2017, 3,051 eligible patients were recruited and given a simple blood test to check for the presence of the HIV virus, as well as hepatitis B and hepatitis C viruses. Patients were living in rural and urban areas and have been treated in 18 different university and community hospitals across the county, from Montana to Mbadachusetts. The median age was 60.6 years and 60% of the participants were women. Registration in the minority was high; Of the total enrolled patients, 18% were Latino and 18% African American. The most common types of participants in the cancer study were treated for bad, blood, bone marrow, colorectal and lung cancers.
S1204 is also notable for its results. Despite the different oncology practice guidelines on viral screening of cancer patients, there is very little evidence on which to base these recommendations. Ramsey and his team sought to illuminate the debate about universal screenings in the cancer community by understanding the prevalence of HIV and hepatitis in newly diagnosed patients.
[ad_2]
Source link