[ad_1]
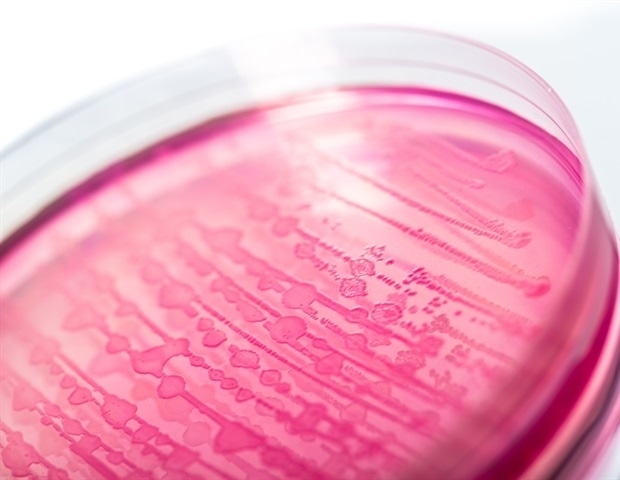
A recent study of more than 1,000 healthy women with no symptoms of urinary tract infections showed that nearly 9% had multiresistant Escherichia coli strains in their intestines.
This is a clinical concern because the E. coli bacteria, responsible for the disease, can pbad from the digestive tract to the female urinary tract via the urethra, the urinary tract, which is shorter and positioned differently in women. The bacteria can then enter the bladder and other parts of the urinary tract.
More than one-third of the urine samples provided by those who had a fluoroquinolone-resistant (Cipro) -resistant digestive tract E. coli tested positive for E. coli growth. Of these, nearly 77% were resistant to Cipro and the clonal type of the bacteria matched the fecal sample.
Most pathogens E. coli found belonged to the ST131- multiresistant pandemicH30R or ST1193 clonal groups that currently cause the majority of urinary tract infections and drug-resistant bloodstream. They were detected twice as often in the urine of people with these strains in the intestine, compared to other strains of E. coli in general.
In addition, the presence of ST ST131-H30R in the intestine in this study was badociated with older age.
The researchers also verified which participants had possibly received a prescription for antibiotics during the study for any type of infection, including respiratory.
Three months after this urine collection, urinary tract infections were diagnosed in almost 7% of the 45 previously asymptomatic carriers who consented to the follow-up examination of the electronic medical record. Participants in the study came from the Puget Sound area.
"The two pathogenic strains of the urinary tract resistant to pandemic fluoroquinolone E. coli discovered in clinical specimens are higher intestinal colonizers and tend to persist there, "the researchers noted. They may also appear, at an unusually high rate, in the urine of healthy women who did not have a documented diagnosis at the time of the sample test. Both phenomena seem to be interconnected.
The researchers pointed out that it has long been known that a patient's microbial flora often hosts strains causing urinary tract infection. It was not certain that pandemic drug-resistant strains have distinct mooring patterns in the gut or lower urinary tract of healthy people.
The study was published in the Oxford University Press, Clinical Infectious Diseases.
The findings could have several implications in terms of clinical care and infection control, according to Evgeni V. Sokurenko, a professor of microbiology at the University of Washington's School of Medicine. He was the principal investigator of the study.
Several other microbiology professors from UW and researchers from the Kaiser Permanent Research Institute in Seattle have collaborated on this work. The principal investigator was Veronika L. Tchesnokova, Department of Microbiology, Faculty of Medicine, University of Medicine.
Results suggest specific resistance to several drugs E. coli the strains detected in this study have a much longer residence in the intestine than some other resistant strains, and can also become present in the urine of healthy women without causing burns, emergency , blood in the urine or other warning signs of a bacterial infection.
Sokurenko explained that whether multidrug-resistant strains are present in a woman's intestine could help predict the resistance pattern of a subsequent clinical infection. Efforts to eliminate the pandemic strains of E. Coli in the intestines of carriers could reduce their rates of multidrug-resistant infections and possibly protect their household or other contacts.
Sokourenko also said the drugs may need to reexamine the clinical significance of the discovery of bacteria in the urine, even without symptoms, during this pandemic of multiple antibiotic resistant strains. E. colibecause these strains could expose carriers to a bacterial disease that is difficult to treat.
Fluoroquinolones are the most commonly prescribed drugs for urinary tract infections. Despite efforts to limit its use, strains resistant to this category of antibiotics are in full swing and are spreading worldwide, according to the researchers.
The superior capacity of the two pandemic strains, ST131-H30R and ST119, installing long-term in people's guts, may have contributed to their rapid global spread, the researcher said. They can be maintained and transmitted in healthy individuals even in the absence of the use of antibiotics, which can disrupt the microbial composition of the intestinal flora.
The researchers concluded that this study highlights the likely physiological reasons for the pandemic of these resistant bacteria. E. coli strains. It also emphasizes the value of determining the carrier status of patients to predict future resistant infections, and the need to rethink the clinical significance of bacteria present in the urine without symptoms, d & # 39; as much as these pandemic strains can be superbugs: highly pathogenic. to the urinary system and resistant to treatment.
National Institutes of Health grants supported this research. Sokurenko has filed patent applications for the detection of E strains. Coli and is one of the leading shareholders of Genomics ID.
Source:
Journal reference:
Tchesnokova, V.L. et al. (2019) Escherichia coli resistant to fluoroquinolone and pandemic uropathogens have an increased ability to persist in the intestine and cause bacteriuria in healthy women. Clinical Infectious Diseases. doi.org/10.1093/cid/ciz547.
[ad_2]
Source link