[ad_1]
An immune hyper reaction, called a cytokine storm, due to the uncontrolled release of an excessive amount of cytokines has been reported as a major contributor to multi-organ dysfunction in SARS-CoV-2 infection.
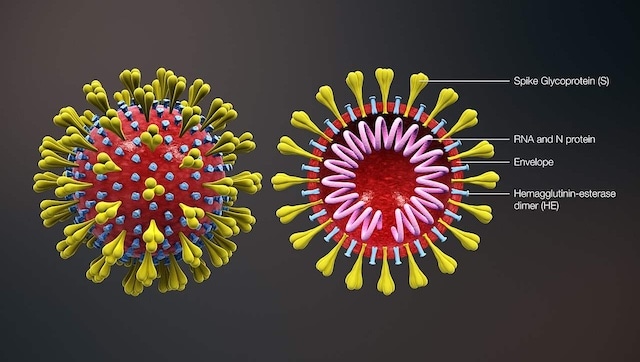
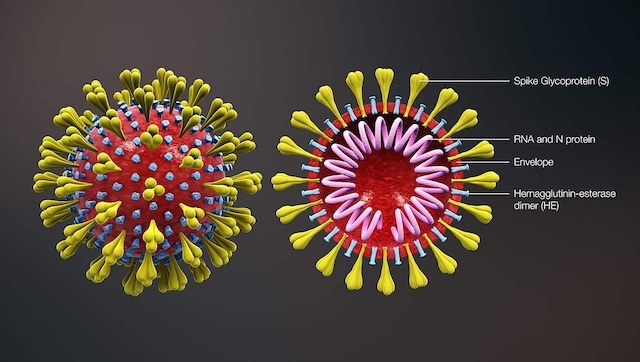
The structure and sectional view of the human coronavirus. It shows the shape of the coronavirus as well as the cross-sectional view. The image shows the major building blocks, including Spike S protein, HE protein, viral envelope, and helical RNA. Image credit: Wikipedia
This happens a year since the first case of COVID-19[female[feminine has been detected and a worrying trend among COVID-19[female[feminine
has been detected and a worrying trend among COVID-19[female[feminine patients are noticed. Some of them return to hospital with post-COVID-19 pulmonary fibrosis. Pulmonary fibrosis refers to the scarring of lung tissue and is associated with permanent pulmonary architectural distortion and irreversible pulmonary dysfunction.
patients are noticed. Some of them return to hospital with post-COVID-19 pulmonary fibrosis. Pulmonary fibrosis refers to the scarring of lung tissue and is associated with permanent pulmonary architectural distortion and irreversible pulmonary dysfunction.
Typically, pulmonary fibrosis is caused by severe lung injury secondary to respiratory infections, chronic granulomatous diseases, drugs, and connective tissue disorders. Available clinical, radiographic and autopsy data have indicated that pulmonary fibrosis is central to the pathology of Severe Acute Respiratory Distress Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) and current data suggests that Pulmonary fibrosis could also complicate infection with SARS-CoV-2.
Pulmonary fibrosis COVID-19[female[feminine
Fibrosis could be seen as the consequence of a disorderly healing process. Various mechanisms of lung injury in patients infected with SARS-CoV-2 have been described, with viral and immune mediated mechanisms involved. An initial phase of lung injury is followed by acute inflammation as well as attempted repair. This process can lead to the restoration of normal lung architecture or it can lead to pulmonary fibrosis with architectural distortion and irreversible lung damage. An immune hyper reaction, called a cytokine storm, due to the uncontrolled release of an excessive amount of cytokines has been reported as a major contributor to multi-organ dysfunction in SARS-CoV-2 infection.
Certain risk factors have been identified as predisposing to pulmonary fibrosis post-infection with SARS-CoV-2. These include advanced age, a history of smoking, severe illness, a prolonged stay in intensive care, and mechanical ventilation. Mechanical ventilation poses an additional risk of ventilator-induced lung injury (VILI), which can lead to pulmonary fibrosis.
Elevated serum lactic acid dehydrogenase (LDH) levels during illness are correlated with post COVID 19 sequelae (residual complication or disease state). Serum LDH has been used as a marker of disease severity after acute lung injury and is an indicator of lung tissue destruction. The mechanisms by which SARS-CoV-2 infection causes pulmonary fibrosis are not fully understood, but pulmonary fibrosis mediated by transforming growth factor-b (TGF-b) and L-converting enzyme angiotensin 2 (ACE2) are among the best documented.
Long term effects
A substantial proportion of patients who develop ARDS will have long-term residual impairment of lung function and HRCT (high resolution computed tomography) signs of pulmonary fibrosis. These patients end up with permanent lung damage to varying degrees and may require home oxygen supplementation for an extended period of time, even after recovery from a COVID 19 infection. Therefore, the role of anti-inflammatory drugs in the disease. Treatment of moderate to severe infections cannot be waived, especially in patients requiring oxygen, where steroid use has shown definite mortality benefit.
The role of available anti-fibrotic therapies like pirfenidone and nintedanib (which are used for the treatment of idiopathic pulmonary fibrosis) in preventing or reducing post-COVID fibrosis, is under evaluation. They promote broad antifibrotic activity, regardless of etiology, and these drugs may have a role in attenuating pro-fibrotic pathways in SARS-CoV-2 infection. The burden of fibrosing lung disease after infection with SARS-CoV-2 is likely high; therefore, given the scale of the pandemic, the global burden of fibrotic lung disease is likely to increase dramatically in the times to come.
This article was written by Dr Richa Sareen, Consultant, Respiratory and Critical Care Medicine, Fortis Hospital, Vasant Kunj, New Delhi.
For more information, read our article on COVID-19[female[feminine and permanent lung damage.
and permanent lung damage.
The health articles in Firstpost are written by myUpchar.com, India’s first and largest resource for verified medical information. At myUpchar, researchers and journalists work with doctors to bring you information on all things health.
Source link