
[ad_1]
Researchers investigating attitudes towards the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) vaccination among the UK population found that, overall, most people were willing to accept a vaccine.
The SARS-CoV-2 virus is the causative agent of the current 2019 coronavirus disease pandemic (COVID-19) which continues to pose a significant threat to global public health and the global economy.
The study also found that certain subgroups of the population were unlikely to accept a vaccine (reluctant to vaccinate), which has important implications for public health policy, according to the team.
Analysis of nationally representative survey data revealed that 82% of participants were likely to accept a vaccine. However, women, younger people, and people with less education were more likely to hesitate to immunize.
Certain ethnic groups, particularly blacks, Pakistanis and Bangladeshis, were also more likely to be reluctant to be vaccinated.
The team – from the University of Glasgow, the University of Essex, Public Health Scotland and Ipsos MORI UK Ltd – said the main reason for the reluctance to vaccinate was concern about unknown future effects.
As the UK is rolling out a vaccination program, these findings have important implications for steps to increase adoption, the researchers say.
“Herd immunity may be achievable through vaccination in the UK, but a focus on specific ethnic minorities and socio-economic groups is needed to ensure a fair vaccination program,” writes Michaela Benzeval (University of Essex ) and his colleagues.
A pre-printed version of the paper is available on the medRxiv * server while the article is subject to peer review.

A safe and effective vaccine is essential to control COVID-19
Large-scale administration of an effective and safe SARS-COV-2 vaccine is crucial to bringing the COVID-19 pandemic under control, but reluctance to vaccinate could undermine those efforts.
Ideally, the proportion of the vaccinated population would be large enough that those who are not vaccinated are also protected (this is called herd immunity).
Knowing whether certain subgroups are more likely to accept or decline a vaccine is critical to designing effective vaccination strategies to achieve herd immunity.
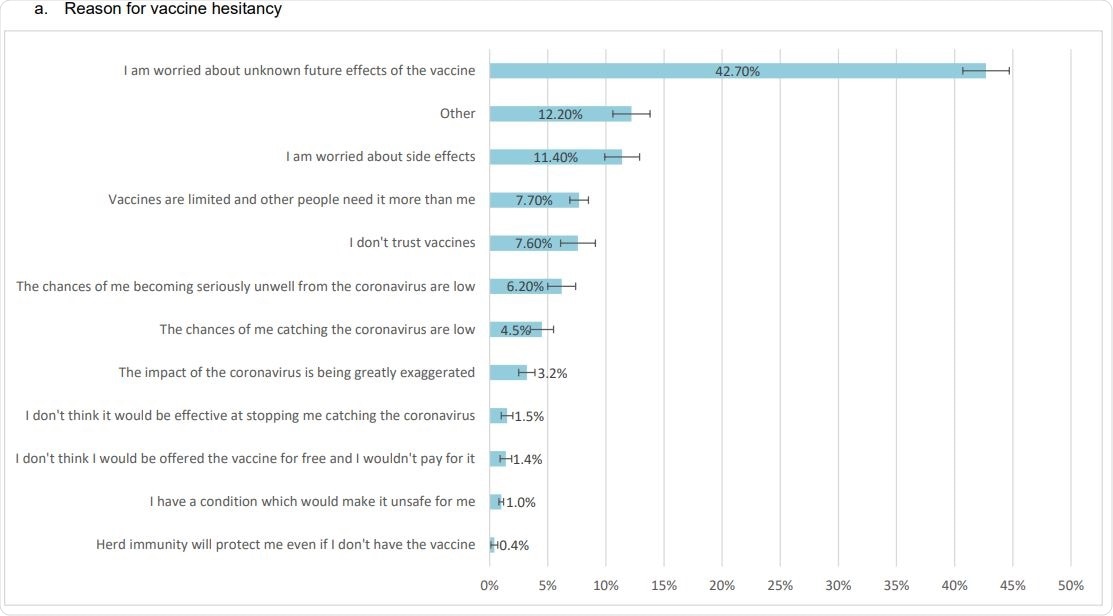
Reasons for hesitating to get vaccinated, willingness to get vaccinated, and factors that might persuade people to get vaccinated (proportions weighted with 95% CI bars)
What did the researchers do?
Nationally representative data available for 12,035 people participating in wave 6 of the COVID-19 “Understanding Society” online survey was collected from 24e November to 1st December 2020.
Participants were asked how likely or unlikely they would be to receive a vaccine and the reasons why.
“The four UK countries are rolling out a vaccination program starting with those most at risk of death from COVID-19,” the team writes. “The findings reported here provide evidence on which groups need targeting and arguments that may be most compelling to them.”
Hesitation varied considerably between subgroups
Overall, the intention to be vaccinated was high, with 82% of respondents saying they were likely (28.5%) or very likely (53.5%) to have a vaccine. However, 18% said it was unlikely or very unlikely to receive the vaccine.
The intention to be vaccinated varied considerably between population subgroups.
A higher proportion of women reported reluctance to vaccinate than men, at 21.0% versus 14.7%, and a higher proportion of younger age groups indicated reluctance to vaccinate, compared to older groups.
Among those aged 16 to 24 and those aged 25 to 24, vaccine reluctance was 26.5% and 28.3%, respectively. This compares to 14.3% among those 55 to 64, 8.1% among those 65 to 74 and just 4.5% among those 75 and over.
“Older age and being male are the biggest risk factors for death from COVID-19, they are less likely to be reluctant to be vaccinated, which suggests that the vaccination program could bring great health benefits to the UK, ”said Benzeval and his team.
Reluctance to immunize also varied significantly by ethnicity, with black (71.8%) and Pakistani / Bangladeshi (42.3%) being the most hesitant, followed by those of mixed ethnicity ( 32.4%) and white non-British / Irish people (26.4%). .
People with less education were also more likely to hesitate to vaccinate. Among graduates, 13.2% said they were reluctant to vaccinate, compared to 24.6% of those with GCSE and 18% of those without qualifications.
Overall, the top reported reason for reluctance was concerns about unknown future side effects from a vaccine, with 42.7% citing this as the reason.
The main reasons for wanting to be vaccinated were to avoid catching the virus or becoming very sick (54.6%) and to allow social and family life to return to normal (12.5%).
The study also found that knowing that a vaccine is effective and safe were the main factors that would encourage uptake of the vaccine.
What are the implications of the study?
“Our study has important practical implications for public health policy,” the team writes.
The risk of vaccine hesitation varies widely between ethnic minority groups in the UK, with black, Pakistani and Bangladeshi groups being particularly likely to be reluctant to vaccinate, the researchers say.
“People with less education were also more likely to hesitate to vaccinate,” they add.
Benzeval and his colleagues say vaccine reluctance is a complex problem and that a series of practical steps must be taken to increase uptake.
“The subgroups that we have identified as hesitant to immunize should be included in the planning and development of any engagement program,” they conclude.
*Important Notice
medRxiv publishes preliminary scientific reports which are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or treated as established information.
Source link