[ad_1]
Cardiac arrests outside the hospital triggered by an opioid overdose are a leading cause of death in adults aged 25 to 64, according to a science release from the American Heart Association, the nation’s largest voluntary health organization focused on heart and brain health for all.
The statement published today in the Association’s flagship journal Circulation.
In the United States, opioid use disorder affects approximately 2 million people each year and costs more than $ 78 billion in health care.
The opioid epidemic, which spans more than three decades, was responsible for an estimated 128 deaths per day in 2018, mostly among adults aged 25 to 55. And more than 15% of opioid overdose cases in emergency medical services in 2016 included cardiac arrest.
Out-of-hospital cardiac arrest associated with opioids differs from other forms of cardiac arrest in how it abnormally affects bodily functions and the different ways it presents itself.
Opioids include prescription drugs, as well as hospital-only non-medical and synthetic opioids like heroin and fentanyl, respectively. In opioid use disorder, they are frequently mixed with alcohol or other toxic substances, increasing the risk of overdose.
Cameron Dezfulian, MD, FAHA, senior author and vice chair of the Scientific Statements Editorial Group, said: “This evidence-based review is valuable in helping to improve the prevention and treatment of out-of-hospital cardiac arrests associated with opioids, which predominantly affects people in their prime. And there is important scientific evidence to consider since this type of cardiac arrest is fundamentally different from sudden cardiac arrests outside the adult hospital, which have been more often studied. “
The scientific statement defines the unique characteristics of cardiac arrest associated with opioids, explains how bodily functions are affected, and provides advice on treatment options.
Dezfulian, who is a senior professor of pediatric critical care medicine at Baylor College of Medicine and medical director of the ICU Adult Congenital Heart at Texas Children’s Hospital in Houston, explains that in cardiac arrests associated with opioids, hypoxia (deficiency of oxygen) occurs before the heart. stops and has important implications for brain damage.
Without oxygen, the brain is damaged within minutes before the heart even stops.
These findings underscore the need for further research to understand and appropriately treat these complications that result from opioid-associated cardiac arrest, particularly potential brain damage and the possible use of treatments that can protect the brain.
Naloxone, an urgent first treatment for overdose, can quickly and effectively reverse respiratory depression or hypoventilation caused by opioids.
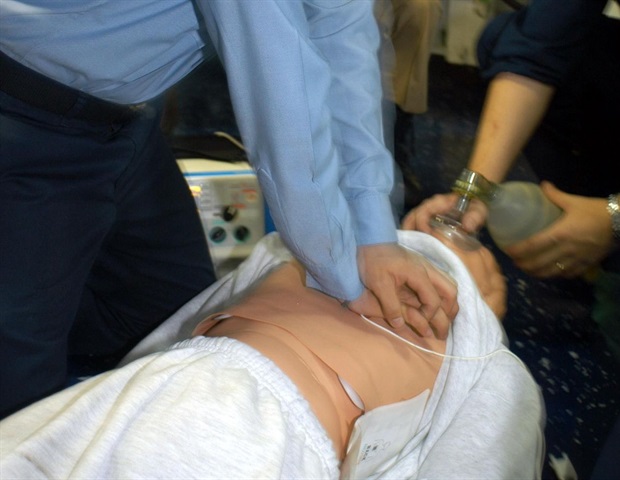
Emergency medical responders, trained laypersons, and the general public (with the support of instructions from the 911 emergency dispatcher) can administer naloxone to prevent cardiac arrest. Traditional CPR, including airways and artificial respiration, can also be effective.
Yet, people who experience out-of-hospital cardiac arrest associated with opioids are more likely to be alone at home or in a private setting – away from someone who witnesses the first signs of cardiac arrest and takes action. There is also evidence of underreporting due to the stigma associated with opioid poisoning and the potential for criminal charges for others in possession of opioids.
Optimizing outcomes after cardiac arrest associated with an opioid overdose requires recognition of the distress by another person – the lay public or emergency dispatchers, prompt emergency response, and treatment with naloxone or CPR ventilation associated with compressions.
Cameron Dezfulian, MD, FAHA, lead study author and vice president
Prompt use of naloxone may prevent progression from respiratory arrest to cardiac arrest; improving access to this life-saving drug is one way to prevent cardiac arrests associated with opioids.
Since opioids often stay in the body for several days, patience is essential in trying to predict results. The statement recommends delaying decisions about stopping rescue efforts until there has been time for the drugs to be cleared from the patient’s system, especially until:
at least 72 hours after the return of spontaneous circulation and normothermia (normal body temperature); toxic substances and their metabolites were eliminated, and sedatives and pain relievers in intensive care were eliminated. Education can be another essential part of the fight against opioid overdoses and out-of-hospital cardiac arrests associated with opioids.
“Targeted educational campaigns providing information on prevention and education on opioid use disorders, naloxone distribution and training in conventional CPR, including artificial respiration, to those at risk of having or witnessing an opioid overdose could help prevent and improve treatment of out-of-hospital heart disease associated with opioid arrest, ”Dezfulian said.
“Along with wider public awareness, legal reforms and policies to prevent opioid-associated cardiac arrests can save lives and should include resources for drug therapy to improve recovery for a generally young segment. of our otherwise healthy population.
Source:
American Heart Association
Journal reference:
Dezfulian, C., et al. (2021) Out-of-hospital cardiac arrest associated with opioids: Distinctive clinical features and implications for healthcare and public responses: A scientific statement from the American Heart Association. Circulation. doi.org/10.1161/CIR.0000000000000958.
Source link