[ad_1]
Of all the coronaviruses that can infect humans, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is the virus responsible for 2019 coronavirus disease (COVID-19), has been recognized as the most infectious. . Other coronaviruses that have caused outbreaks include Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV). Usually, these viruses infect the respiratory tract and cause pneumonia-like symptoms.
The novel SARS-CoV-2 was first reported in Wuhan, China in December 2019. Subsequently, due to mutations, several variants of SARS-CoV-2 such as Alpha, Beta, Delta variants and Gamma appeared.
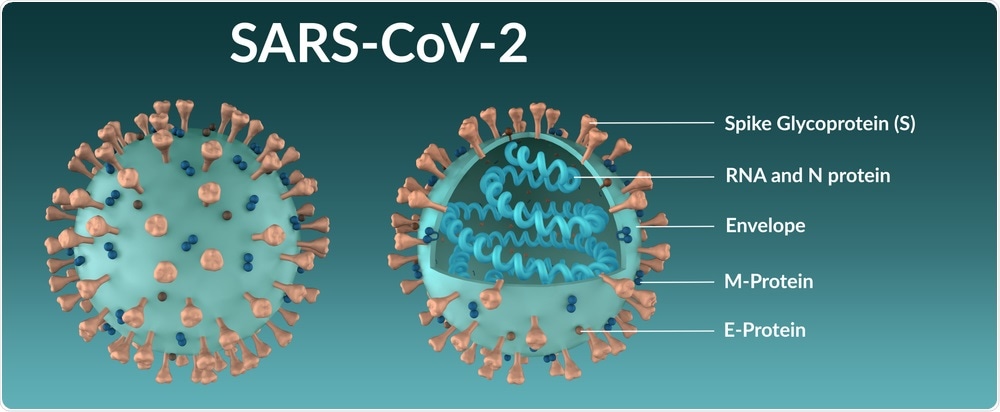
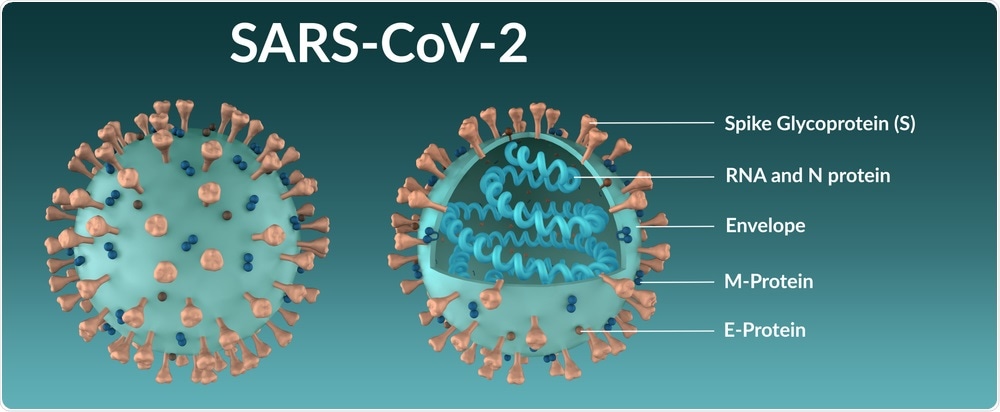
The genomic sequence of SARS-CoV-2 has led to the identification of four structural proteins, including spike (S), membrane (M), envelope (E) and core (N) proteins, as well as other non-structural proteins and accessory proteins.
All COVID-19 vaccines that have received Emergency Use Clearance (EUA) from various federal regulatory agencies around the world are based on the S protein due to its crucial role in SARS infection- CoV-2.
How does SARS-CoV-2 infect cells?
The SARS-CoV-2 protein mediates viral entry inside the host cell. The S protein contains two domains which include S1 and S2.
The S1 domain consists of receptor binding domains (RBD) that bind directly to the angiotensin converting enzyme 2 (ACE2) receptor, which is present on the cell surface of the host. Comparatively, the S2 domain contains the fusion peptide which allows fusion of SARS-CoV-2 to cell membranes.
Several changes occur at the molecular level after viral invasion to allow this virus to control the host’s cellular mechanisms and initiate viral replication. Since the binding of RBDs to ACE2 plays a key role in viral pathogenesis, inhibition of this binding could prevent viral infection.
Traditional medicinal plants and viral infection
Plant extracts containing different secondary metabolites possess various medicinal properties, such as antimicrobial and antispasmodic activity, with minimal side effects. For example, thyme was once used for the treatment of asthma, laryngitis, colds, and throat congestion. In the 16th and 17th centuries, wild thyme was used for the treatment of malaria and epilepsy. The Balkans also used thyme as an anti-cholesterol lowering and immunostimulant.
Another interesting immunomodulatory property of thymol is that it can improve the expression of the cytokines CD4, CD8 and Th1 through the upregulation of the expression of interferon 4 (IFN-4). This agent can also stimulate the secretion of interleukin-12 (IL-12).
Emodin is another phytocompound that acts as an inhibitor of the 3a ion channel of the SARS-CoV and HCoV-OC43 coronaviruses. Previous studies have also found that high concentrations of emodin can inhibit different stages of the virus’s life cycle.
A new study
Considering the antiviral activity of herbal remedies, a new study published in the journal Current pharmacology reports focuses on identifying potent phytochemicals from Himalayan herbs, namely, Rheum emodi, Serpyllum thyme, and Artemisia annua, for the treatment of COVID-19.
Here a in silico approach demonstrated the potential of unique phytocompounds (emodin, thymol and carvacrol) to bind the S-glycoproteins of SARS-CoV-2 (6VXX and 6VYB), the S-glycoprotein of the B.1.351 variant, as well as with ACE2. These phytocompounds could also prevent the binding of SARS-CoV-2 to the host ACE2, TMPRSS2 and neutrapilin-1 receptors.
Chloroquine has already been used for the treatment of COVID-19. For this reason, the authors compared the binding pattern of chloroquine and artemisinin with S proteins (6VXX, 6VYB) and its 7NXA variant, to understand its mode of action and inhibitory effects.
In this study, researchers used AutoDock / Vina software to identify phytochemicals that could bind to S protein. These molecular docking studies screened many phytocompounds and reduced them to emodin, which showed the better binding affinity with 6VYB and the SARS-CoV-2 B.1.351 (7NXA) variant. Emodin also showed the best interactions with TMPRSS 2 and ACE2.
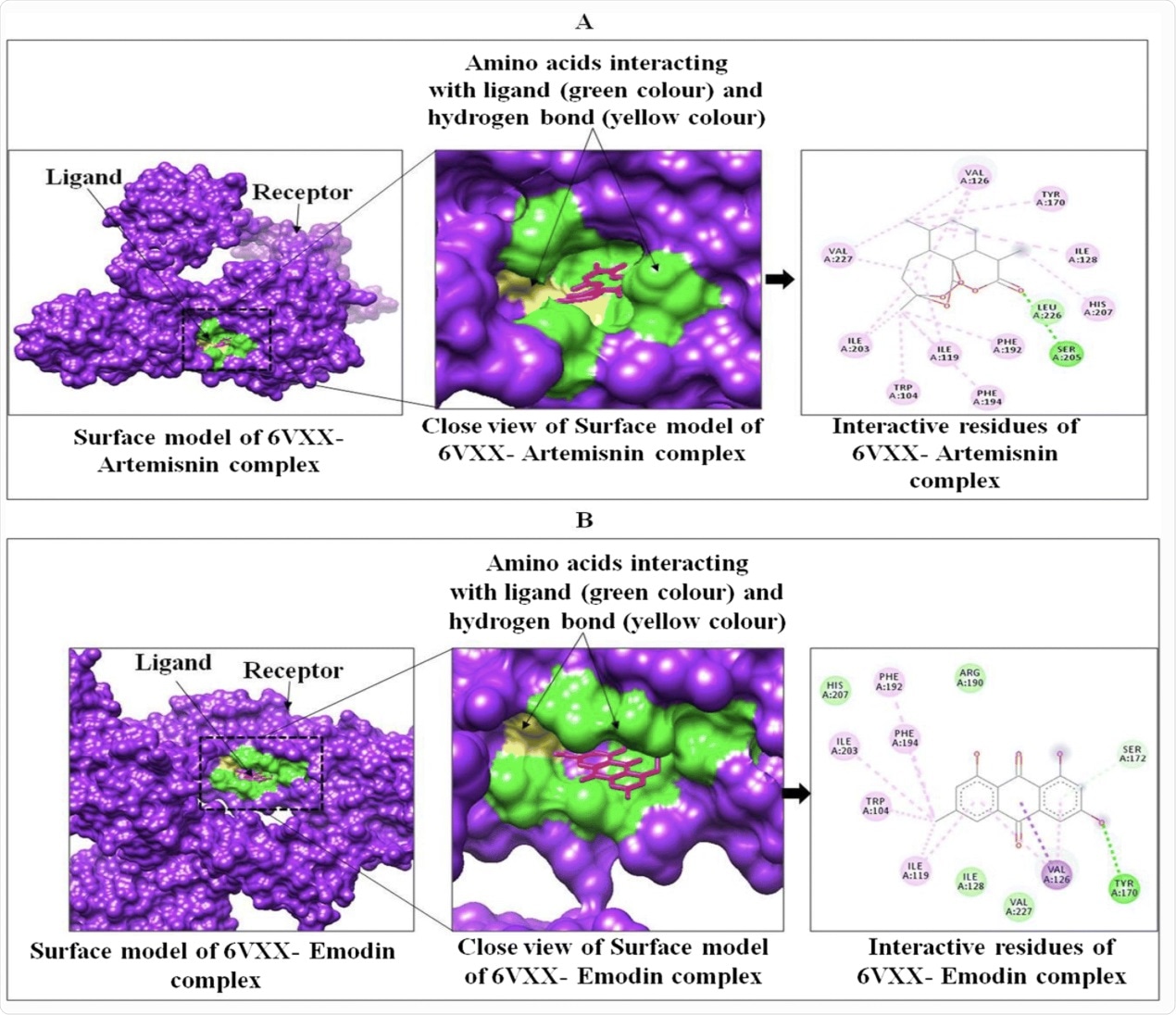
Interactions between SARS-CoV-2 Targeted Protein Receptor Spike Glycoprotein (PDB ID: 6VXX) with Artemisinin (A) and Emodin (B) using Chimera.
In this study, although the lowest binding energy was observed in artemisinin with 6VXX and 6VYB, this compound showed a significant interaction with TMPRSS 2 and ACE2. Molecular dynamics (MD) simulation was also performed for 50 ns. In the Ramachandran plot developed after MD, the two S protein domains exhibited less than 1.0% aberrant amino acid residues.
Overall, the MD simulation study found that the interaction of artemisinin with 6VYB compared to 6VXX was more stable. The researchers also found that all of the plant compounds evaluated in this study are non-toxic and non-carcinogenic.
Conclusion
In view of these results, the authors recommend artemisinin as a potential phytocompound that can effectively inhibit the interaction between SARS-CoV-2 and the ACE-2 receptor, especially when the S protein is in an open state conformation. .
The current research is unique in that it compared the open (6YVB) and closed (6VXX) conformations of S proteins. Interestingly, the open state of S protein (6YVB), which was found to be more pathogenic, showed a more stable interaction with artemisinin compared to the closed state (6VXX).
To come up in vitro and in vivo studies should be conducted to determine the therapeutic efficacy of artemisinin for the treatment of COVID-19.
Source link