[ad_1]
With the end of the government's closure and the beginning of Congress's stance on rising drug costs, the news cycle is once again full of heartbreaking stories about how the cost of insulin hurts patients and their families. The first fact lost in the translation is that insulin does not refer to one, but to several different drugs and is probably the first miracle drug that has extended the quantity and quality of life in an extraordinary way. Insulin is a sort of collateral damage related to the price war of medicines, a chimeric revelator for the better and for worse of the pharmaceutical industry.
The basics
Insulin regulates the amount of glucose, sugar, in the blood, acting in opposition and in collaboration with glucagon. It is released by the pancreas when the blood glucose level rises, forcing the sugar into the cells where it is converted into energy. Type I diabetes affects the youngest patients and is thought to result from an infection or allergic response to their own islet cells, the source of insulin – these patients are dependent on insulin. Type 2 diabetes is more of a relative insulin deficiency that develops later in life, in combination with dietary choices and exercise, among other factors. Although patients with type 2 diabetes can take insulin, they are more likely to take medications that "activate me". [1] and stimulate the production or enhance the effect of the patient's own insulin.
History of insulin
Similar to penicillin, insulin originated in a Canadian doctor, Frederick Banting, an orthopedic surgeon who developed a line of research, suggested by another scientist, that the pancreas held the key to glucose metabolism. He formed a rather uneasy alliance with a skeptical physiologist, John Macleod, who provided the lab, dogs, and a medical student, Charles Best. Their work led to the discovery of insulin and Banting and Macleod were awarded the Nobel Prize in Medicine; Banting remains the youngest recipient of this award. A biochemist, James Collip, was asked to improve performance and eliminate impurities from insulin, from the dog pancreas; contaminants that caused irritation and adverse effects in the first human patients. It has not been able to convert laboratory techniques into industrial production methods and Eli Lilly has taken over the torch by putting insulin on the scale.
The patent that Banting, Best and Collip were cited for the process of insulin isolation and purification was handed over to the University of Toronto for three dollars.
"A patent was needed to limit the manufacture of insulin to reputable pharmaceutical companies, able to guarantee the purity and potency of their products. This would also prevent unscrupulous drug manufacturers from making or patenting a powerless or weakened version of this potentially dangerous drug and calling it insulin. " [2]
During his visit to the United States, August Krogh, another Nobel Prize-winning physiologist, accompanied by his wife's doctor, herself suffering from type 2 diabetes, got the # 39; authorization to bring insulin to Scandinavia. The couple joined a company pharmacist who funded the creation of an institute to extract insulin from animal pancreas. The institute has grown to Novo Nordisk, a global pharmaceutical giant that spends 85% of its efforts on treating diabetes.
For the next 50 years, until the early 1980s, Eli Lilly and Novo Nordisk made the old-fashioned insulin by extracting and purifying pancreas from slaughtered cattle and pigs.
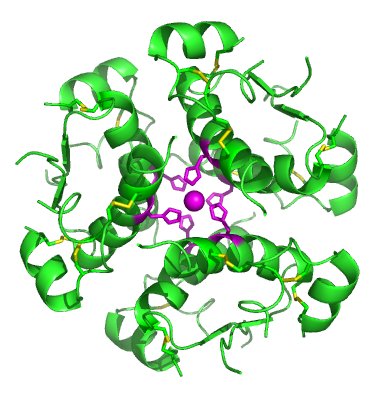
Biochemistry of insulin
Insulin is a unique molecule, consisting of two peptide chains linked together by three chemical bonds. Proinsulin, the precursor molecule of insulin, consists of two chains and another segment that "transports" proinsulin to an area of the cell where both insulin chains are bound and the carrier segment is removed. These nearly complete bademblies with a small cap remaining, consider it a security lock on a firearm, are then moved into storage granules, where the "trigger lock" is removed. The insulin is then stored in groups of six, maintaining their structure while remaining inactive until it is called and released from the granules; groups of six who separate and insulin now fully active act in this way.
Insulin is a biological molecule whose complexity makes synthesis difficult. Insulin was the first biological product and held this distinction for many years. Today, many expensive companions are used to treat other autoimmune diseases, such as irritable bowel syndrome or rheumatoid arthritis, drugs priced at $ 100,000.
Scaling up production
The fact that cows, pigs and some fish have an insulin structure very similar to ours allowed us to harvest insulin from these creatures. Eli Lilly found that the quality and quantity of insulin available in beef and pork pancreas varied and worked hard to isolate insulin to eliminate impurities causing adverse reactions, but to increase the yield so that that insulin can be used by a growing number of patients. patients in need.
In the late 1970s, the insulin gene was identified and the first genetically modified insulin was created in 1982 using genes inserted into a bacterium or yeast. Yes, insulin that this vital drug is the product of a GMO. Today, insulin production on an industrial scale follows one of the two following routes. The DNA used to form the two chains of insulin or to create proinsulin is inserted into bacteria or yeasts that raise the synthesis, the resulting chains or proinsulin being isolated and bound or separated. These GMO products are considered synthetic "human" insulin.
The action of insulin keeps our blood sugar levels in a certain range and the mere fact of giving insulin to a patient can not mimic the feedback mechanism of our body. [3] this allows a careful titration to avoid hyperglycemia that is too high or too low (hypoglycaemia). The synthetic human insulin eliminated some of the insulin-like variation of animal origin with adverse effects, but it could not replicate the release of insulin by our pancreas. To try to mimic these actions and produce insulin that further reduced the adverse moments of too high and above all too low blood sugar, scientists again changed human insulin by creating like. These slight alterations of the amino acid sequence of insulin [4] provide reliable short- and long-term actions. Lispro, an "badog insulin," is rapidly absorbed and ultra-short-acting, while glargine, another badogue, is released relatively consistently over a 24-hour period, causing neither peak nor trough.
It remains an important controversy whether these new, more expensive insulins produce better results than slightly older synthetics. But there is compelling evidence that, for patients, these insulins are often easier to take and that respect for medication is always an advantage.
The price of insulin
First, it should be clear that insulin as a complex biological product is more difficult to synthesize, which requires the intervention of natural means adapted to our scientific will. As a biological product, its competitors are not generics, but biosimilars. You can find a more meaningful discussion about biosimilars and generics here. In summary, biosimilars face higher regulatory hurdles and costs, while their cost is lower than the original biologic, well beyond the savings you make with a generic version of a simple chemical compound. . As a general rule, biosimilars sell for 20% less than branded ones; in the generic world, the reduction is generally closer to 80%.
Three companies supply insulin worldwide, the two original manufacturers, Eli Lilly and Novo Nordisk, and the French conglomerate Sanofi, whose many acquisitions included a company producing glargine, a slow release insulin to be administered once a day. . As for all highly concentrated and quasi-monopoly producers, the price of their products, in this case insulin, increases most often. It is difficult to identify what are the new costs leading to price increases that lead to higher prices: insurance companies, forms and co-payments.
Given the controversy surrounding whether new, more expensive insulins produce better clinical results than slightly older synthetic insurance companies, they would prefer to pay for cheaper drugs. To encourage patients to obtain these drugs, they invented various techniques; New drug co-payments are higher and not all of the newer medicines are on the form and are not available at all. In other cases, you must use a cheaper version before you can even pay the higher co – payment, a technique called step therapy. In other cases, the doctor must justify his choice of the most expensive drugs, with prior authorization.
Pharmaceutical companies struggle in terms of both manufacturing and price. The original patent sale on insulin priced at $ 3 is over, altruism has been replaced by the fiduciary responsibility of listed companies to generate a profit for their investors. Manufacturers dragged on their feet, not providing drug samples to companies wishing to create biosimilars, they tried to extend their patent protection, including trying to transfer patents to an American tribe , whose "sovereign" rights would override US patent law (though ingenious). , the case failed).
In terms of price, manufacturers offer discounts on "the advertised price" to insurance companies and directly to patients. This results in a lack of transparency in drug pricing because the price paid is unknown to all parties. If a drug is 60% discounted by a wholesaler, the drug does not guarantee that these savings will be pbaded on to patients. . The selling price of a medicine is an initial offer in the price negotiation; patients are involved as a source of all payments and consequential damages in this failing market. It failed for various reasons, but the display of the price of the sticker, the average wholesale price, is as useful to buy drugs as the price recommended by the manufacturer for the purchase of a car.
Insulin is not a drug, insulin is composed of many drugs. This is the poster of a medical miracle and a market failure. It goes back to our past and, in some ways, predicts our future.
[1] Trulicity's slogan [2] Insulin: discovery and controversy [3] Although the road is made in an artificial pancreas [4] These changes are similar to those that CRISPR-Cas9 technologies can achieve, but were developed 30 years ago and did not benefit from the accuracy of CRISPR.Source link