[ad_1]
They might be dubbed ‘windows to the soul’, but the COVID-19 pandemic has reinforced the fact that the eyes are also ‘portals of infection’. Using MRI, radiologists see significant optical abnormalities in patients who have suffered from severe viral illness.
Unusual eye findings have been reported in patients infected with COVID-19 in the early stages of the pandemic – even before China declared its initial emergency. But, as providers largely focus on life-threatening aspects of the illness, these issues are often overlooked.
Although the virus is known to primarily attack the lungs, impacts on the eye have been detected, including conjunctivitis, chemosis, optic neuritis, and retinopathy. But, to date, little research has been published on what the virus can actually do to the eyes. In a study published on February 16 in Radiology, researchers from the French Society of Neuroradiology (SFNR) presented the first ocular MRI results associated with COVID-19.
To learn more about what the virus does, the team recruited 129 patients from 11 universities and five general hospitals between March 4, 2020 and May 1, 2020. Six patients were obese and two patients each had diabetes and hypertension. All patients had severe viral infection and the team performed 1.5 T of 3T brain MRI on each participant.
For more coverage based on knowledge and research from industry experts, subscribe to the electronic diagnostic imaging newsletter here.
“We have shown that a few patients with severe COVID-19 in the French COVID-19 cohort had one or more nodules from the posterior pole of the globe,” said lead author Augustin Lecler, MD, Ph.D. ., associate professor at the University of Paris and neuroradiologist at the Adolphe de Rothschild Hospital Foundation in Paris.
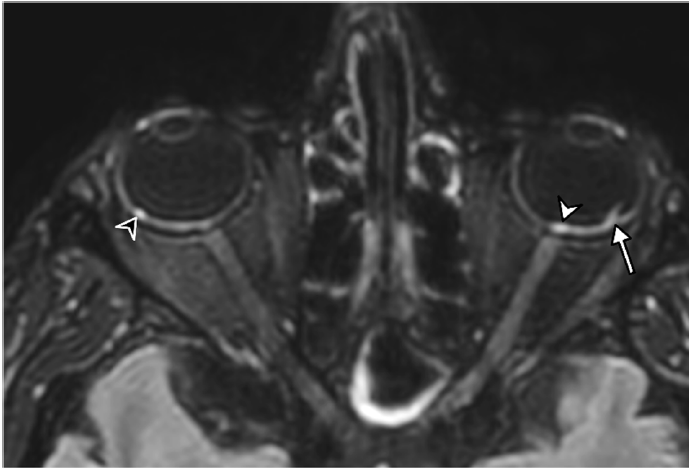
Of the 129 patients – 43 women and 86 men – nine (7%) had an abnormal MRI in the eyeball, the team said. All nine patients had nodules in the macular region, the area of the eye responsible for central vision. Eight patients had nodules in both eyes. Two had nodules outside the macular region.
In addition, one patient had multiple infarctions in the territory of the anterior cerebral artery; one had a frontal hematoma; one had multiple micro-hemorrhages from the splenium of the corpus callosum; and one had leptomeningeal enhancement without parenchymal abnormalities. No patient presented with abnormalities of the optic nerve, optic chiasm or optic tract.
These results do not shed light on the mechanism behind the formation of the nodules. However, Lecler said, his team has several hypotheses around the root cause. The inflammation triggered by the virus could be the cause. Previous literature has reported that human coronaviruses can cause retinitis, choroiditis, retinal detachment, or optic neuritis. Another cause could be inadequate drainage of the eye veins caused by lying face down in the intensive care unit or being intubated for long periods of time. Seven of the affected patients had long-term ICU admissions.
While it’s unclear what causes these eye abnormalities to develop, Lecler said, these results still point to the need to screen patients who have had severe COVID-19 to detect any potential nodules.
“Our study calls for screening all ICU hospital patients for severe COVID-19,” he said. “We believe that these patients should receive specific eye protection treatments.”
Screening efforts could include the use of high-resolution MRI to explore the eyes, as well as fundoscopy and optical coherence tomography.
According to Claudia FE Kirsch MD, division chief of neuroradiology and professor of neuroradiology and otolaryngology at the Zucker Hofstra School of Medicine in Northwell, this study is important because it draws attention to a complication of COVID-19 which has been largely overlooked.
“It is essential to remember that eye problems may not be recognized in the ICU, and clinicians should be vigilant in first identifying if there is an orbital problem to protect the patient’s vision,” he said. she declared. “Awareness of a new discovery, disseminating this information and sharing with colleagues leads others to recognize the problem, educate, research, understand and improve results.”
The study, she said, is a reminder to radiologists to pay attention to eye sockets on MRI scans, especially with COVID-19 patients in ICUs.
And that research is ongoing, Lecler said. His team is performing follow-up clinical and MRI exams on all COVID-19 survivors to determine if they have long-term clinical consequences, such as loss of vision or visual field impairment. Additional MRI assessments, coupled with more comprehensive ophthalmologic testing, are also underway for an next group of patients with both severe and moderate infection from the second and third waves of the pandemic.
“We have initiated a prospective study with dedicated high-resolution MRI images to explore the eye and orbit in patients with mild to moderate COVID,” said Lecler. “Therefore, we will be able to know whether our results were specific to a severe COVID patient or not.”
Source link