
[ad_1]
During prenatal ultrasounds or birth, many new parents look between their baby's legs: the presence of a penis is a strong sign that it is a boy.
For humans and other animals, it was believed that penile development was dictated by the "male hormones" (androgens) entirely produced by the testes of the male fetus during its growth in the uterus.
However, a new document released today indicates that this might not be the case. Some of the masculinizing hormones that stimulate penile development may come from other sources of the developing fetus. These include the liver, the adrenal glands (small glands on the kidneys) and the placenta.
For the first time, this work exhaustively examines possible hormone production sites outside the testes and their role in regulating masculinization – the process of obtaining typical male characteristics. This helps us to see how we develop as embryos and could allow us to better understand why penis development disorders are increasing.
Read more:
Our relationship with dick picks: it's complicated
Testosterone is not enough
The penis develops from an embryonic structure called bad tubercle or GT.
GT is present in men and women and develops in clitoris or penis, depending on its exposure to hormones secreted by developing gonads (ovaries or testes).
In females, developing ovaries do not produce early hormones and the GT becomes feminized by forming a clitoris.
In men, developing testes produce testosterone. This circulates in the developing fetus and causes masculinization of the target tissues and induces penis development from the GT.
Testosterone itself is a relatively weak hormone. It is converted in the penis into another hormone called dihydrotestosterone (DHT), which has a much more powerful masculinization effect.
It is the local conversion of testosterone into DHT in the tissue that is important for penile development and other changes.
The fetus can make DHT in several ways. The simplest is the testicular testosterone conversion (the so-called "canonical" pathway). However, DHT can also be produced via other steroidal hormone pathways active in many tissues, which is deepened in this new article.
Read more:
What makes you a man or a woman? The geneticist Jenny Graves explains
Common birth defects
Understanding the pathways that control penile development is important. Disorders affecting penile development are among the most common conbad anomalies observed in humans. The hypospadias (disorder affecting the development of the urethra) currently affects about 1 in every 115 Australian-born men, and rates are increasing.
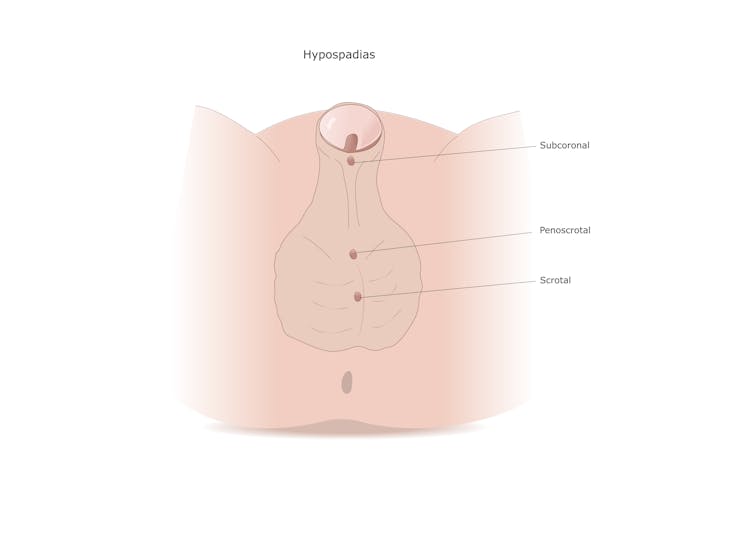
from www.shutterstock.com
In fact, the incidence of hypospadias has doubled in the last 40 years. Such a rapid increase in incidence has been attributed to environmental factors, with endocrine disrupting chemicals (EDCs) being proposed as a major cause. EDCs are synthetic chemicals used in many industries – for example, in the production of plastics, cosmetics, flame retardants and pesticides. They can interfere with the hormonal and metabolic systems of our body.
Of the 1,484 EDCs currently identified, a large number negatively affect the development of male reproduction.
Numerous studies have identified the harmful effects of PE on organs, such as the liver and adrenal glands, resulting in diseases and disorders that affect the health of these organs and disrupt human development.
Doorway
By measuring hormones from blood and tissue samples during the second trimester of human fetal development, this new research helps us understand the pathways that lead to the production of DHT and masculinization of the penis.
This suggests that in addition to the canonical pathway (testosterone testis converted to DHT in the GT and motor penis development), male steroids are synthesized by other organs, such as the placenta, the liver and adrenal gland through a process called 'backdoor'. "Way to contribute to masculinization. The backdoor trail was discovered for the first time through research conducted here in Australia on marsupials.
The results of this research suggest that EDC could have effects on non-reproductive tissues, including the adrenal glands and liver, and then cause reproductive diseases in humans, such as hypospadias.
In addition, this indicates that placental defects, such as intrauterine growth restriction which causes babies to be born small, could contribute to male reproductive diseases in humans.
Further research is now needed to track these interesting findings in order to explore possible new causal pathways for disorders that begin during pregnancy.
Source link