[ad_1]

Treating a patient effectively involves both training and experience. This is one of the reasons that the prospects for using AI in medicine elicit enthusiasm: it is possible to train algorithms using the experience of thousands of doctors and providing them with more information than any human being could accumulate.
This Week Has Provided Some clues suggest that software could live up to this promise, two documents describing excellent preliminary results using AI for diagnosis and treatment decisions. The articles address very different issues and approaches, suggesting that the range of situations in which IA could be useful is very broad.
Choice of Treatments
One of two studies deals with sepsis, which occurs when the immune system mounts excessive response to an infection. Sepsis is apparently the third leading cause of death in the world and remains a problem even when the patient is already hospitalized. There are recommendations for the treatment of patients with sepsis, but the figures suggest that there is still much to be done. A small US-UK team decided to see if any software could help bring some of this improvement.
They used a reinforcement learning algorithm because this one is considered effective when there is what they call "rare reward signals". In other words, such a large patient population will have many other problems than sepsis, which will largely influence treatment outcomes, so that the signal of effective treatments will be weak and difficult to achieve. detect. This approach was intended to increase the chances of detecting one.
Just as the large number of data points used to train the software: more than 17,000 patients in intensive care unit and 79,000 other admissions to the hospital in a total of more than 125 hospitals. Patient data included 48 different information, from vital signs to laboratory tests to demographic information. The algorithm used the data to identify treatments that could maximize patient survival at 90 days. The researchers called the software obtained Clinician AI.
A separate set of patient records was used to evaluate the performance of the AI clinician. The algorithm was used to choose a treatment and the patients were evaluated according to the similarity of their treatments with those recommended by the algorithm. Overall, the software has recommended lower doses of intravenous fluids and higher doses of drugs resulting in constriction of blood vessels. People who received treatments similar to these recommendations had the lowest mortality among this group of patients.
Diagnosis
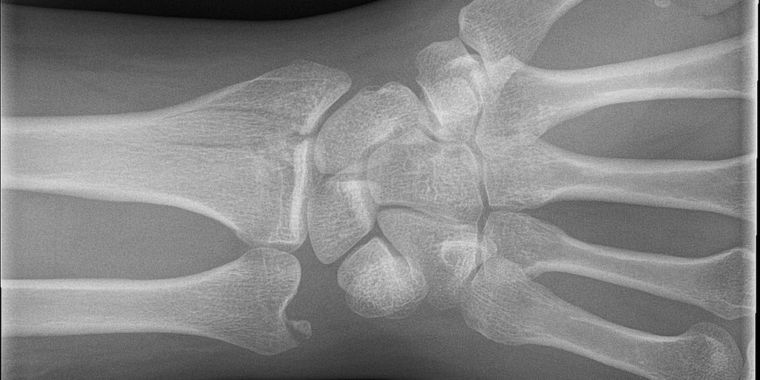
The second document dealt with the identification of problems requiring treatment. The problem on which bone fractures are concentrated. Although they are often easy to spot, even a specialist can hardly detect small fractures caused by scales or wicks. And, in most cases, the diagnosis goes to a non specialist, usually a doctor working in emergency medicine. The new research is not aimed at creating an AI that replaces these doctors;
The team recruited 18 orthopedic surgeons to diagnose more than 135,000 images of potential wrist fractures, and then used this data to form their algorithm, a convolutive neural network with deep learning. The algorithm was used to highlight areas of interest for non-orthopedic physicians. Basically, it helped them focus on areas that might contain breaks.
In the past, trials like this have resulted in overdiagnosis, in which doctors recommended additional tests for harmless treatments. But in this case, accuracy increased as false positives decreased. Sensitivity (or ability) to identify fractures increased from 81% to 92%, while specificity (or the ability to make the correct diagnosis) increased from 88% to 94%. Together, these results mean that ER physicians have had their misdiagnosis rate drop by almost half.
Neither of them used the software in a context that fully reflected the medically relevant circumstances. Emergency physicians and those who treat sepsis (who may be one and the same person) will normally have many additional concerns and distractions. It can therefore be difficult to incorporate the use of AI into their process. But the success of these efforts suggests that AI clinical trials will take place sooner than planned, and we will then have a clear idea of their contribution to diagnosis and treatment.
Nature Medicine 2017. DOI: 10.1038 / s41591-018-0213-5 (About the DOIs).
PNAS 2017. DOI: 10.1073 / pnas.1806905115 (About DOIs).
Source link