
[ad_1]
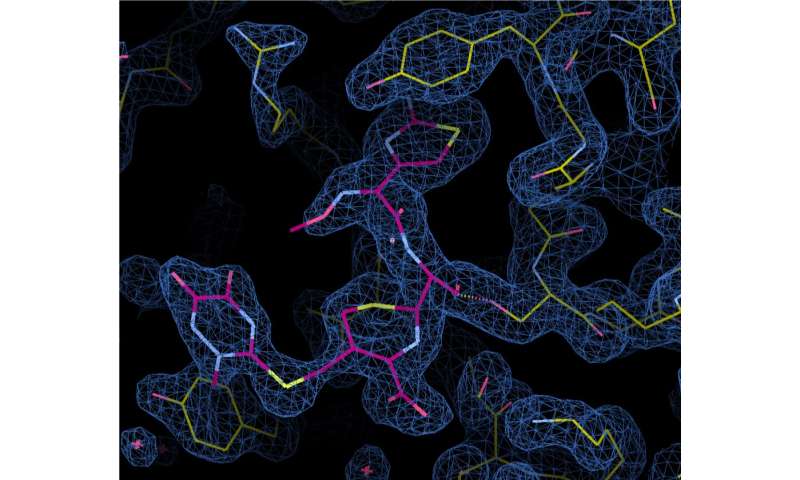
This image generated by X-ray crystallography shows a cephalosporin antibiotic, in pink, binding to a protein of the bacterium responsible for gonorrhea. Spheres represent molecules of water. Credit: MUSC
Steadily and relentlessly, the bacterium that caused gonorrhea has surpassed the defenses of medicine and acquired resistance to previously reliable drugs, including penicillin, tetracycline and ciprofloxacin. These old pillars are no longer used to treat sexually transmitted diseases.
In 2010, after a few strains of Neisseria gonorrhoeae, the bacterium responsible for gonorrhea, has begun to show resistance to one of the last classes of antibiotics, Centers for Disease Control and Prevention have begun to recommend "dual therapy", which means that doctors prescribe now two drugs at the same time to fight against gonorrhea. Currently, these two drugs are ceftriaxone, a member of the cephalosporin antibiotic class, and azithromycin.
With growing fears that gonorrhea may violate these latest defenses, the work of researchers such as crystallographer Christopher Davies, Ph.D., is crucial.
"We are looking at events that are of concern to everyone at molecular level clinics," said Davies, a professor in the Department of Biochemistry and Molecular Biology and Director of the MUSC Structural Biology Center.
The Davies team has just published an article showing how cephalosporins bind and inactivate a gonococcal protein called penicillin-2 binding protein (PBP2). Under the direction of Avinash Singh, a postdoctoral doctorate, the researchers showed that the protein was undergoing important structural changes, including a twisting and winding of a loop to bind the body. antibiotic, which improved the reaction with cephalosporins. Without these changes, the protein would react much more slowly with the antibiotic.
Davies explained that all antibiotics act by targeting the essential functions of a particular bug. Cephalosporins act by attacking the bacterial cell wall.
Normally, PBP2 moves along the cytoplasmic membrane of the bacterial cell, reaching the gap between the cytoplasmic membrane and the outer membrane, looking for peptides to bind to. Protein connects peptides to create a net, just like an onion bag at the grocery store, Davies said. But antibiotics jump to bind to the protein before it can reach a peptide.
"The protein normally circulates around the membrane layer, but its active site is blocked by an antibiotic, so that all potential interactions with the peptide substrate are unsuccessful," said Davies.
With the protein out of order and not building the mesh, holes begin to appear in the cell wall. The cytoplasm begins to leak and the cell bursts and dies, Davies said.
Yet resistant strains identified in Japan, France, Spain and more recently Canada escape the lethal action of cephalosporins by preventing the antibiotic from binding to the target protein. How they do it is one of the main goals of Davies' research.
There are about 60 mutations of the PBP2 protein in resistant strains of gonorrhea. The Davies team has identified six mutations that are at the basis of resistance and examines how these mutations alter how the protein reacts to antibiotics.
Once researchers understand how mutations prevent antibiotics from doing their job, new drugs can be developed, Davies said. Knowing what mutations are important can also help develop a diagnostic test that tells doctors if a particular patient has a resistant strain and, therefore, which drugs to prescribe.
Davies said that it appeared that the mutations restricted the flexibility of the protein, thus preventing the structural changes needed to bind the antibiotic. This triggers a new mystery. If these movements are essential to its work of binding to peptides and building the mesh that keeps the cell wall intact, how can the mutations block the antibiotic while allowing a normal reaction? "It's the most fascinating aspect of our research," Davies said.
"This is an essential function, so that the mutations can not alter the protein too much, it must be able to discriminate, discriminate an antibiotic while maintaining the normal binding and the reaction with its substrate is a delicate balance they have to negotiate, "he said.
This balance may be the reason why antibiotic-resistant gonorrhea has not spread as fast as expected.
"There is a cost of fitness.They do not work as well as their likely counterparts, and it is probably for this reason that they do not spread as fast as people feared it", said Davies.
Although resistant-type gonorrhea is not spreading as quickly as public health officials feared, the number of susceptible gonorrhea cases, as well as other sexually transmitted diseases has increased.
Gonorrhea diagnoses increased by 67% between 2013 and 2017, according to the CDC.
"We expect gonorrhea to eventually exhaust our last highly effective antibiotic, and additional treatment options are urgently needed," said Gail Bolan, MD, director of the CDC's STD Prevention Division, when she published these figures.
South Carolina has the fourth highest gonorrhea rate, according to a CDC number analysis conducted by Health Testing Centers, a laboratory testing service.
MUSC's infectious disease specialist Eric Meissner, MD, Ph.D., said that the reason why STD rates were increasing is not entirely clear.
"We know that individuals can use proven interventions, including consistent use of condoms, which significantly reduce the chances of contracting a sexually transmitted disease." The increase in STD rates therefore suggests that he more action and education is needed in public health, "he said.
Although gonorrhea is not fatal, it can cause life-long problems if it is not treated, including infertility and susceptibility to other sexually transmitted diseases, such as HIV. .
"It is important for people to know that you can have gonorrhea and have no symptoms, so you can not rely solely on the absence of symptoms to make sure that you or your sexual partner does not have any symptoms. you do not have gonorrhea, "said Meissner. "Sexually active people at risk of exposure to gonorrhea should be subject to regular testing".
Meanwhile, Davies and his team continue their lab work. The next step is to understand how protein can still perform its essential function while avoiding antibiotics. The group has some ideas that it will put to the test, he said.
Meissner said antibiotic resistance was a concern for the clinic's doctors.
"Even though the specific strain being studied by Dr. Davies is rare, it's important to note that the onset of resistance to gonorrhea is a real concern," Meissner said.
Scientists develop test to identify best treatment for gonorrhea
Avinash Singh et al., Recognition of β-lactams Carboxylates Triggers Acylation of the Penicillin 2 Neisseria gonorrhoeae Binding Protein, Journal of biological chemistry (2019). DOI: 10.1074 / jbc.RA119.009942
Quote:
Researcher seeks to understand how gonorrhea develops resistance to antibiotics (23 Aug. 2019)
recovered on August 23, 2019
https://phys.org/news/2019-08-gonorrhea-resistance-antibiotics.html
This document is subject to copyright. Apart from any fair use for study or private research purposes, no
part may be reproduced without written permission. Content is provided for information only.
[ad_2]
Source link