[ad_1]
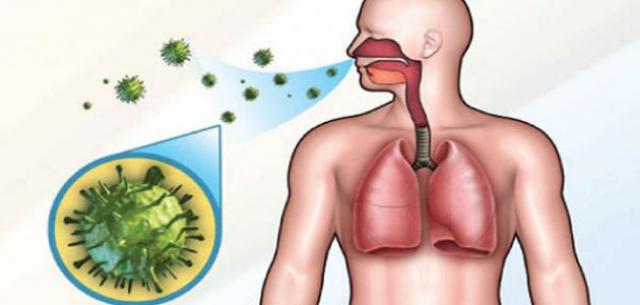
The most common respiratory diseases in the respiratory system in humans. Information on SARS Information on inflammation of the chest
Tuberculosis is a disease caused by a bacterium called Mycobacterium tuberculosis. It usually attacks bacteria and lungs. It can also attack other parts of the body and spread the TB bacteria in the air when a person has tuberculosis and starts to cough or sneeze or to sneeze. personal conversations. Where people are closest to each other and where people who are vulnerable to immunity are most vulnerable to TB, this article discusses the types of TB and their symptoms, as well as their causes, as well as the diagnosis and treatment possible.
Types of tuberculosis
The medical community divides tuberculosis into two main types depending on whether or not there is active tuberculosis and active tuberculosis: about one third of the world's population would suffer from latent tuberculosis, with a 10% chance that passive tuberculosis becomes active, In immunocompromised, HIV-infected or malnourished people or smokers, TB affects all age groups around the world. Yet the disease often affects young people and people living in developing countries. And in 2012 shows that 80% of the reported TB cases have appeared in only 22 developing countries. Here is an overview of the types of tuberculosis categorized by doctor:
Severe tuberculosis: in this case, the body is infected with tuberculosis, but the bacteria present in the patient's body remain inactive and cause no symptoms (latent tuberculosis, noninfectious disease, but it can turn into tuberculosis). It is therefore important that the person with underlying TB undergo treatment to control the disease and reduce the spread and treatment of the disease.
Active TB: The state in which the symptoms appear in the patient, who can start transmitting the disease to others who live there, and can occur in the first few weeks of TB infection or occur after years.
Symptoms of tuberculosis
Although pathogenic bacteria are present in the body in all types of TB and its conditions, the immune system can prevent the disease and is therefore divided by type of TB as follows:
Symptoms of underlying tuberculosis
During the period of inactivity of the disease, the patient shows no symptoms, because of the inability of bacteria to attack the body members through the protection provided by the body's immune system.
Symptoms of active tuberculosis
In case of disease activity, the bacterium of tuberculosis attacks the lungs and causes severe lung tissue damage, resulting in the following symptoms:
The cough lasts for three weeks or more and may be accompanied by blood.
Chest pain, often associated with breathing, laughing, coughing or sneezing.
Anorexia, which results in unplanned weight loss in most cases.
Fever, night sweats, exhaustion and fatigue.
Chills with feeling cold most of the time.
Symptoms of non-pulmonary tuberculosis
Tuberculosis can affect organs other than the lungs, including the kidneys, brain, spine and bones. In non-pulmonary tuberculosis, the signs and symptoms vary depending on the affected organ. The infected bones, while cerebral tuberculosis causes various psychotic and neurological symptoms, such as hallucinations, headaches and others.
Causes of tuberculosis
Mycobacterium tuberculosis is caused by tuberculosis and there are various strains of bacterial tuberculosis, some of which are drug-resistant, and the bacterium of tuberculosis passes through the droplets coming out of the human mouth. When this spray comes out of the mouth of an infected person, it can be inhaled by his loved one. By the breath or cough Transient bacteria can cause both types of TB and the underlying TB may become active over time, or more particularly at a time when the immune system is weak.
Risk factors for tuberculosis
In some cases, such as those that cause systemic weakness or various environmental factors, the risk of tuberculosis increases:
Immune Weakness in the Human Body: In most cases, immune system cells are able to suppress the bacteria from TB and prevent them from harming the body's organs. Thus, in cases of low immunity, bacteria find an appropriate opportunity to invade the body and cause damage, and in some cases weaken the immune system in the body.
HIV infection or so-called AIDS.
Diabetes.
Chronic renal failure.
Some types of cancer or chemotherapy.
Certain immunosuppressive drugs used in the treatment of certain immunological diseases such as Crohn's disease and psoriasis, or administered before transplantation.
Malnutrition, whether for lack of food sources or pollution.
Older people or young people because of their vulnerability to immunity.
Travel to certain areas: Tuberculosis is more serious when traveling or traveling to affected or under-served areas, including African, East Asian, African, Middle East and North African countries. Eastern Europe and Latin America.
Poverty and lack of health care: Poverty and the difficult physical condition of human disability can provide access to necessary medical care.
Smoking Smoking is known to have a negative effect on the body's immune system, increasing the risk of complex diseases such as cancer and tuberculosis.
Place of work or accommodation, for example:
Work in health care facilities: Since health care providers must deal directly with patients with TB, the risk of bacterial transmission increases, so wear masks and protective gloves.
Presence in hospital care facilities: The risk of infection is higher in places of overcrowding such as prisons and old people's homes.
Living in camps: due to malnutrition, lack of health care and poor environmental conditions.
Diagnosis of tuberculosis
Tuberculosis must be diagnosed as quickly as possible because of its impact on the speed of treatment, it must also aim to reduce the spread of the bacteria responsible for the disease and include tests and diagnostic tests, as follows:
Skin test: The doctor can use the PPD to determine if a person has tuberculosis and inject 0.1 milliliters of PPD – a small amount of protein – under the top layer of the skin and after two or three days if the area is red or red. Swelling and swelling greater than 5 mm at the PPD injection site is a positive test result. The positive result indicates that the patient has tuberculosis, but can not determine whether the disease is active or latent, and swelling of 5 to 15 mm can be considered positive, as appropriate. Risk factors, health and medical history of the patient, However, the results of this test are not considered final: some patients do not show test response despite the disease, while others respond to the test without TB It should be noted that people who have recently received the TB vaccine may have a positive skin test because of the presence of the vaccine in the blood.
Blood tests: the doctor may request blood tests in monitoring the results of the tuberculosis analysis. Blood testing may be preferable to skin testing in certain health conditions or in specific groups of people. Some tests for tuberculosis have been approved recently:, Blood test results are positive, negative or indeterminate, such as skin tests, and blood tests can not determine whether tuberculosis is active or not.
Chest X-ray: If the skin or blood test is positive, it is likely that an x-ray is used to pull on the chest, which looks for a few small dots in the lungs. These patches, if any, are a sign of TB infection and the body tries to isolate them. TB means that the patient has active TB and should start treatment, but if the result is negative, TB is likely to be latent or the results of previous tests are inaccurate.
Other tests: the doctor may also ask for mucus or mucus tests taken from the depths of the lung to check for the presence of tuberculosis. If the mucosal tests are positive, it means that the disease is active and can spread, and must therefore wear a special mask even after treatment can be started until the phlegm test becomes negative, then the mask may be removed.It may be necessary to perform other tests, such as a chest CT scan, bronchoscopy or lung biopsy, if the other test results remain unclear.
Treatment of tuberculosis
Because of the extreme risk of tuberculosis, it can be fatal if it is not treated, but the risk of death is very low if the patient receives appropriate treatment and the situation, and most patients do not get treated. do not need to be treated in the hospital, as many think, Q:
Treatment of active pulmonary tuberculosis
Active TB is treated with the requirement to take a number of antibiotics for six months.The patient is often infectious during the first treatment period.It can run out several weeks before the patient The exact time depends on his general health and the severity of tuberculosis, After taking antibiotics for two weeks, the patient is not prepared for others. However, it is important to continue taking the medications as planned and complete the full antibiotic treatment. Treatment for six months is the best way to kill TB bacteria. Vital Antagonist Before completing the course or skipping a dose, TB bacteria may become resistant to antibiotics, and is considered very dangerous because it can be difficult to treat and it will take a longer path for treatment using different treatments and may be more toxic, and include the TB treatment plan as follows:
Two antibiotics – isoniazid and rifampicin – for six months.
Two additional antibiotics – pyrazinamide and ethambutol – during the first two months of treatment.
If the treatment is completed properly, the patient will no longer need another TB specialist and may be warned of some signs that may indicate recurrence of the disease, although this is rare.
Treatment of extracellular tuberculosis
Tuberculosis, which occurs outside the lung, can be treated with the same combination of antibiotics that is used for the treatment of pulmonary tuberculosis. If a person has tuberculosis in areas such as the brain or sac heart steroids, such as prednisolone, may be prescribed for several weeks. In addition to antibiotics, this will help reduce inflammation in the affected areas and, as in the case of pulmonary TB, it is important to follow the treatment as planned and complete the entire cycle, even if the patient feels better .
Treatment of underlying tuberculosis
If the patient has underlying tuberculosis, treatment is usually recommended, but it should be noted that antibiotics used to treat tuberculosis can cause liver damage, especially in the elderly.If liver injury are a concern, the medical team will discuss the state of the disease in terms of The priority is to preserve the liver, especially in patients with risk factors for liver disease.In addition, Tuberculosis is not always treated if the bacteria is considered anti-drug. If this is the case, the patient is regularly monitored to verify that the infection is not active. For people who have John with a treatment that would weaken their immune system, such as long-term steroids, chemotherapy or biological inhibitors such as TNF inhibitors, because the risk of underlying tuberculosis activation was high, and treatment for latent TB usually involved either the combination of rifampicin and isoniazid for three months, or isoniazid alone for six months.
Side effects of treatment
Some drugs used to treat various types of TB cause uncomfortable side effects. The isoniazid antibiotic can cause nerve damage – peripheral neuropathy – the patient must then receive vitamin B6-pyridoxine supplements to reduce these risks. The liver before the start of treatment, and in rare cases, can cause antibiotics used to treat tuberculosis damage to the eye, which can be dangerous, and if the patient's treatment plan contains the Ethambutol, must also test the patient's vision at the beginning of the treatment, Rhivam reacts Lysine with other drugs, so it is important that the doctor all drugs covered by the patient before the start of TB treatment.
Prevention and prevention of tuberculosis
The patient will be contagious for a period of two to three weeks from the start of treatment and will not normally need to be isolated during this time, but it is important to take some basic precautions to avoid spreading. tuberculosis to his family or his entourage.
Stay out of work, from school or college until the patient's TB treatment team indicates that their return is safe.
Cover your mouth when you cough, sneeze, or laugh permanently, carefully dispose of used towels in a sealed plastic bag.
Open windows where possible to ensure a good supply of fresh air to areas where the patient spends some time.
Do not sleep with other people in the same room or nearby, because of the risk of spreading the bacteria during sleep unconsciously of the patient.
[ad_2]
Source link