
[ad_1]

Here is the list of what Laura Marston sacrificed to stay alive: her car, her furniture, her apartment, her retirement fund, her dog.
At 36, she has already sold all her possessions twice to afford the insulin that her body needs every day.
Insulin is not like other medicines. It's a natural hormone that controls our blood sugar levels – too high a rate can lead to vision loss, confusion, nausea and possibly organ failure. Too weak causes cardiac irregularities, mood swings, convulsions, loss of consciousness.
For most of us, our body naturally produces insulin. But for Type 1 (T1) diabetics such as Ms. Marston, insulin is supplied in clear glass vials, delivered to the pharmacy counter every month – if they can afford it.
A bottle of insulin that Mrs. Marston uses now costs $ 275 (£ 210) without health insurance.
In 1923, the inventors of insulin sold his patent for $ 1, hoping that the low price would allow all those who need it to benefit from essential treatments.
Today, retail prices in the United States are around $ 300 for all the insulins of the three major brands controlling the market.
Even taking into account inflation, it is about a price increase of more than 1,000%.
Stories of Americans rationing insulin – and dying for it – have made the national newspaper headlines.
The most famous case, perhaps, is Alec Smith, 26, who died in 2017 less than a month after retiring from his mother's health insurance plan. Although he works full time and earns more than the minimum wage, he can not afford to buy new insurance or pay the $ 1,000 a month for insulin without it.

Copyright of the image
Getty Images
Alec Smith's mother holds a vial of her son's ashes at a protest against the high price of insulin in front of the Sanofi offices in Massachusetts
Ms. Marston knows the feeling – like most diabetics I've talked to, she has experienced frightening failures without any fault on her part.
A few years ago, while the small law firm Ms. Marston was working for a brutal closure, she found herself without income and suddenly uninsured.
"I was spending $ 2,880 a month just to stay alive, it was more than I earned even working 50 hours a week," Ms. Marston said.
She was forced to leave her home in Richmond, Virginia, to find a new job in Washington DC in order to pay for insulin.
"I sold everything, including my car, and I had to give up my dog - he was eight and I had to give it – and move to Washington."
There are several reasons why a person is still not insured in the United States – if they do not qualify for insurance offered by their employer or lose their job, such as Ms. Marston, for example, or if she can not afford to pay a plan on her account. own.

Copyright of the image
Laura Marston
"I'm not sure I'll never be able to recover from the pain of having to choose my life instead of living together," says Marston about her dog, Nicky
Ms. Marston was diagnosed with T1 diabetes at the age of 14. She laughs remembering that the price of insulin in 1996 – $ 25 for a bottle – had shocked her.
Two decades later, Mrs. Marston still uses the same insulin formula: Eli Lilly's Humalog. Even the packaging is the same.
"Nothing has changed about this, if it's that the price has gone from $ 21 per vial to $ 275 per vial."
It's the same story for Sanofi's Apidra and Novo Nordisk's Novolog.
So who is to blame?
Most patients point to pharmaceutical companies, which in turn raise issues with government regulations and insurance providers.
At the heart of the problem lies the complex mystery of who pays what for insulin in the United States.

Five terms are essential to the discussion: current price, net price, rebates, share and deductibles.
- List of prices is established by a pharmaceutical company, and in many cases this is what uninsured diabetics pay
- Net price is the real profit that the company receives for a medicine
- Rebates are there discounts on medications negotiated for insurance companies?
- Co-payments are an insured person paying for a prescription, out of his pocket
- franchises, which can reach $ 10,000, are what insurance policies need to be paid before the insurer takes the rest
Insurance companies use third-party negotiators, called pharmacy benefit managers, to set discounts for drug companies, which results in a reduction in the price of the copayment for their users. Experts say the problem with the system is partly a lack of transparency about how these discounts are negotiated and how much is actually charged to patients.
This system also means that insurers are charged different rates for each pharmaceutical company. For example, an insulin brand whose co-payment is minimal under an insurance policy may cost the full price in another.
Ms. Marston has been tracking the current prices of insulin for years. According to her calculations, for insulin alone, it would take her nearly $ 7 million to live up to age 70 if she pays out of her pocket.
"This led to a situation in which I decided that I could not have children because I did not feel financially stable enough," Ms. Marston said.
But drug manufacturers say that very few people are facing list prices.
Eli Lilly said in a statement to the BBC that 95% of people using Humalog in the US pay less than $ 100 a month for their prescription, and that out of 600,000 people using Humalog, "about 1,600 people without insurance n & # Did not use the [assistance] benefits we offer ".
Novo Nordisk and Sanofi have detailed similar patient support programs in their statements. And many diabetics who I spoke to said that these programs helped them if they qualified.

But another lawyer, Kristen Daniels, said she had to pay $ 2400 for a month of insulin and she was technically insured, she could not get help.
"I called my insurance, the manufacturer and no one could help me because I had not reached my franchise," Ms. Daniels said.
Pharmaceutical companies also pointed out that the increase in list prices did not result in corresponding profits. Eli Lilly's spokesman said their net price had dropped over the past five years; Sanofi's said its insulin profits were 25% lower in 2019 than in 2012.
According to a report from the American Diabetes Association (ADA) and the Center for Health Policy and Economics of the University of Southern California, between 2007 and 2016, current prices of leading brands of insulin have increased by 252%, while net prices grew less than 57%. .
And there are cheaper options in the US for some: insulin Walmart, for example, is a renowned version of a Novo Nordisk formula that costs around $ 25 per vial in most states. But the formula is older, less effective and some, like Mrs. Marston, are allergic to it.
This is another key issue in the debate around soaring insulin prices. Each formula works differently for each individual. It takes years for many T1 patients to feel comfortable managing their dosage with a particular brand.
Several diabetics who I spoke with said they were forced to change insulin through their insurance plan – even against the recommendation of their doctor – they wanted to avoid paying the price posted for their favorite brand.

According to the ADA, this "non-medical switching" is more than a drawback: it is potentially dangerous because it requires constant monitoring by the patient and consultations with a doctor.
Serious or permanent complications such as blindness or kidney disease can occur if a diabetic suffers too many highs and lows of extreme sugar levels.
In America, where insurance coverage goes hand in hand with limited options, many T1 diabetics make sacrifices at other times in their lives to continue to pay for insulin – which it's about keeping a stressful job or changing insulin-based formulas at the request of an insurer.
The expression that keeps coming up in the American T1 community is: "We are hostages".

How does the United Kingdom compare?
T1International is a non-profit organization that advocates for affordable and accessible diabetes care around the world. Founder Elizabeth Rowley is an American now living in the United Kingdom.
As a T1 diabetic herself, Ms. Rowley has direct experience navigating both health systems. She describes the American system as "complicated", with profits at all levels.
"People spend most of their lives worrying about losing insurance, running out of insulin and increasing their cost, or having to keep terrible jobs or relationships to make sure they keep their insurance coverage. disease, "says Rowley. "It's the best scenario.
"In the worst case, people are rationing insulin, which has resulted in many deaths and horrible complications." People buy and share insulin from internet users that they have not seen. never met, having to choose between buying food, paying rent or taking their medicine. "
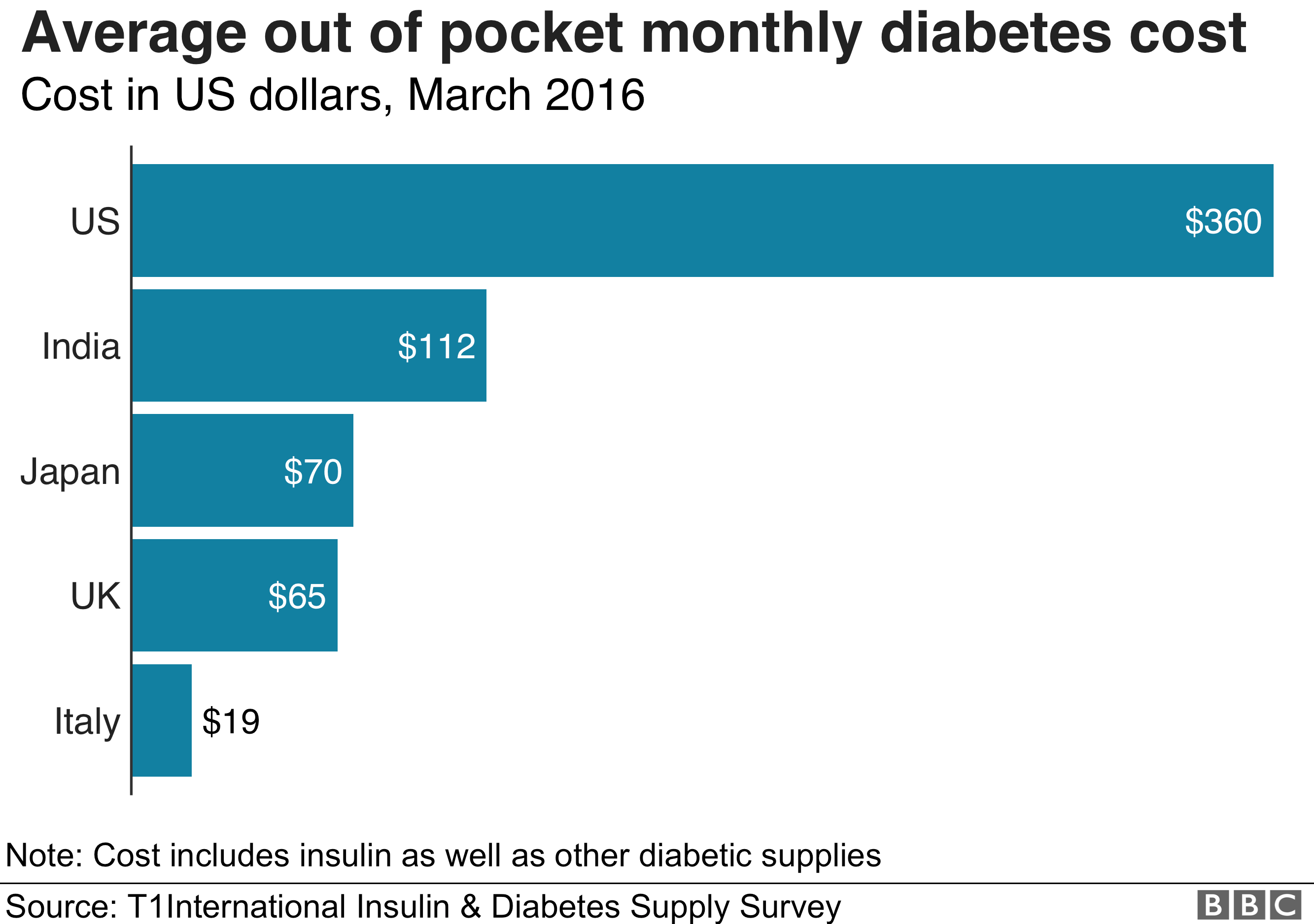
In the United States, diabetics pay an average of more than $ 210 per month for insulin, according to a T1International 2016 survey, compared with less than $ 50 in India or nothing at all in some European countries.
"In the UK, I went into the pharmacy and, with my medical exemption card, I recovered my essential drugs.Although the NHS still pays too much for insulin, its cost is minimal compared what Americans have to pay. "
Rowley acknowledges that these other systems are not perfect – but for her, they are always better for patients.

More voices on health care:


Medical tourists
Lauren Hyre, 30, an Arizona-based T1International lawyer, is very much aware of fears of insulin access in the US system. She struggled with her for two thirds of her life.
His father died at the age of nine and his company terminated the family's health insurance. Before Obamacare, diabetics could be denied insurance, and Ms. Hyre was therefore without coverage for years.
Living in Indiana, a state without expanded health care programs, she also could not claim any government assistance.
For years, Ms. Hyre has relied on outdated insulin bottles from her doctor and on trips to Canada to buy it at an affordable price.
The first time she bought insulin at a Canadian pharmacy, her mother burst into tears.
There are also dozens of similar stories on the other side of the southern border.
When Emily Mackey, 27, heard about a group of diabetics traveling to Tijuana, Mexico, to buy cheaper insulin, she consulted Instagram and joined the group.
His tram ride from San Diego, California to Tijuana, Mexico cost $ 5 round trip. An insulin supply for six months cost her $ 100, much less than the $ 1,300 cost if she was purchased from her insurance.
But his relief quickly turned into aggravation.
"I was angry to have to go to Mexico to get a medicine that keeps me alive." I live right next to one. [US pharmacy], yet obliged to travel 3000 km to another country to get an insulin at an affordable price. "

Copyright of the image
Emily Mackey
Emily Mackey is holding a stack of insulin pens that she bought in Mexico

what are the solutions?
According to the American Diabetes Association (ADA), there are more than seven million diabetics in this country and about 27% of them say that offering insulin has had a affect their daily lives.
Dr. William Cefalu, scientific, medical and mission leader of the ADA, said the lack of transparency was at the root of the problem.
"The system is dysfunctional, there are problems at each level, in every actor in the insulin supply chain," he said. "We can not point to a particular entity."
It is essential to address the issues of high deductibles and to ensure that discounts negotiated with insurance companies are passed on to patients, he said.
Competition would be the best way to lower prices, so why has not it happened yet?
Unlike chemical drugs, which can be simply replicated, insulin is a biological material consisting of proteins synthesized by a cell line specific to each formula.
The insulins of Novo Nordisk, Eli Lilly and Sanofi are all slightly different in this way and no "generic" or unbranded copies can be made without access to the patented materials and processes of these companies.

Flasks containing the last drops of insulin expired that Laura Marston retains as an emergency reserve
Despite these fundamental differences, insulin has long been classified and regulated as a chemical drug.
In December, the FDA announced that the agency would reclassify insulin as a "biologic" by 2020 as part of what the FDA commissioner called a "decisive moment for insulin".
The approval of these so-called biological products will then be easier than before, which will favor the development of "biosimilar or interchangeable products with" existing insulin.
Insulin is not the only drug affected by the entanglement of regulations and closed industrial dynamics, but it is one of the few drugs whose price tag has fatal consequences.
For Ms. Marston, it's hard to see why insulin has already been treated as another medication.
"It's a natural hormone that all other bodies make, but not ours," she says. "There should be price ceilings, like all that is needed for life: your water bill, your electricity bill." It can be said that these things are even less necessary than Humalog. "
As Congress continues to hold hearings on drug prices, drug companies are beginning to feel the pressure.
Eli Lilly has announced that it will offer a new "generic" version of Humalog at a cost two times lower. But the price of $ 137 for this new generic drug remains high – and significantly higher than other countries pay for the same insulin.
This is something that can reduce what some people pay at the pharmacy, but that does not solve the systemic problems of insulin pricing.


Senator Elizabeth Warren, presidential candidate for 2020, and Representative Jan Schakowsky, both Democrats, proposed a different solution in December.
The Affordable Medicines Manufacturing Act would order the Department of Health and Human Services to create a new office specializing in the manufacture of generic drugs "in case of market failure" in order to "revive" competition .
The bill is unlikely to be passed, but some lawmakers are keen that the existing system be changed.
The proposed Medicare for All public plan proposed by Senator Bernie Sanders and other 2020 candidates, which would provide free health care for all, funded by higher taxes.
While the debate continues on Capitol Hill and in the boardrooms of the industry, Ms. Marston said that she wanted to continue to defend her own interests on behalf of those who had failed in the break in the matter. d & # 39; insurance.
"In an instant, they had to pay catalog prices and could not do it, and that's why they died.
"If even a person has to pay the list price, it's not fair," Ms. Marston said.
"It's really someone who has a weapon in his head and who says: Your money or your life."
Photographs by Hannah Long-Higgins
.
[ad_2]
Source link