[ad_1]
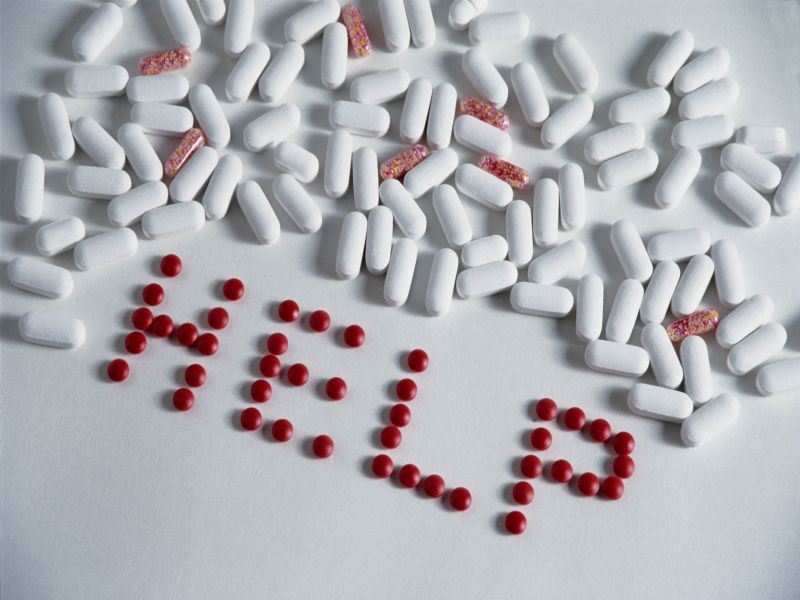
Monday, September 10, 2018 (HealthDay News) – When older people use drugs like Valium or Xanax to calm their anxiety or help them sleep, they are at high risk of becoming addicts, according to a new study.
In the study of nearly 600 adults aged 78 years on average, about one in four who were prescribed these types of sedatives ended up using them for at least one year.
This is despite warnings against the long-term use of medications, especially among the elderly. Benzodiazepines – a class that also includes Ativan, Halcion and Klonopin – can increase the risk of car accidents, falls, broken hips and other harmful side effects, warn experts.
So the new study "shows that we need to help providers start with the prescription of benzodiazepines, starting with a short-term prescription and engaging patients in discussions about when to re-evaluate their symptoms and start reducing the patient ". said the senior author, Dr. Lauren Gerlach. She is a geriatric psychiatrist at the University of Michigan at Ann Arbor.
"We also need to educate providers about effective non-pharmaceutical treatment alternatives, such as cognitive-behavioral therapy, for these patients," said Gerlach in a university press release.
A psychiatrist called the study an indispensable reminder to doctors.
"Clinicians, including psychiatrists, continue to prescribe benzodiazepines [older] the population at an alarming rate, "said Dr. Brian Keefe, medical director of Zucker Hillside Hospital in Glen Oaks, New York.
However, "many studies conducted for many years have consistently shown a high risk of falls and fractures in older people taking these drugs, a risk that increases with the daily dose," said Keefe. .
In the study, the Gerlach team monitored the use of benzodiazepines in 576 elderly people who received their first prescription between 2008 and 2016. Only a few people received psychiatric, psychological or psychosocial care at the clinic. during the last two years, notes the report.
Overall, 152 patients maintained a current or recent prescription one year after initially prescribing a benzodiazepine, according to the study.
The authors explained that the study mainly included people who received their prescription from a primary care physician or another non-psychiatrist because that is how most of the patients older people receive benzodiazepines.
By breaking down the numbers, the Gerlach team found that white patients were four times more likely to use these medications in the long run compared to minority patients.
In addition, people whose initial prescriptions were written for the largest number of pills were more likely to become long-term users. In fact, for an additional 10 days of prescribed medication, the risk of long-term use almost doubled over the next year, the researchers reported.
And compared to short-term users, patients taking long-term benzodiazepines were no longer likely to experience anxiety or depression – two conditions that may warrant long-term use of these drugs.
Long-term users were more likely to say that they had sleep problems, although benzodiazepines are not recommended for long-term use as sleeping pills. In fact, they can even make sleep worse as they are used, according to the researchers.
"As mental health providers see only a very small minority of older adults who have mental health issues, we need to better support primary care providers when they manage care." of these patients, "said Gerlach. "We need to help them think critically about how certain prescriptions they write could increase the chances of long-term use."
So why do so many doctors renew their prescriptions, even if it is not justified?
Keefe had a theory. "Reducing and eventually stopping these drugs can be uncomfortable for both parties," he said. Thus, a reluctance to do so "could result in maintaining the status quo, even if it is not desirable in the long run," Keefe said.
Dr. Harshal Kirane runs addiction services at the Staten Island University Hospital in New York. He called benzodiazepine abuse a "silent epidemic".
The new study "highlights a huge gap between guidelines and real-world practices," said Kirane, and "stresses the ongoing reliance on narcotic medications for the resolution of symptoms such as insomnia, which can be
Mr Kirane said that doctors should do more to help patients with insomnia or other problems to find safer non-pharmaceutical solutions.
The report was published online September 10 in the journal JAMA Internal Medicine.
More information
For more information on benzodiazepines, visit the website of the US National Institute on Drug Abuse.
SOURCES: Brian M. Keefe, MD, Medical Director, Zucker Hillside Hospital, Glen Oaks, New York; Harshal D. Kirane, MD, Director of Addiction Services, Staten Island University Hospital, New York City; University of Michigan, press release, September 10, 2018
[ad_2]Source link