[ad_1]
When you buy raw meat in the grocery store, what you’re bringing home is often more than dinner.
“The chances of you buying a product that is contaminated with drug-resistant-bacteria is very high,” said Dr Lance Price. Price is the Founding Director of George Washington University’s Antibiotic Resistance Action Center, a leading research laboratory at the Milken School of Public Health.
“We raise 9 billion food animals to be slaughtered and made into meat,” said Price. “When we give them low doses of antibiotics on a routine basis, we’re just fueling the growth of bacteria, drug resistant bacteria, that can spread among those animals and then they get distributed to every grocery store in the country.”
It’s estimated that 70 percent of antibiotics used in America are given to farm animals that end up on your dinner plate.
“Food animal producers have to be careful in the way they use antibiotics,” said Price. We can’t just be using them to prevent infections that they’re causing by raising animals in a way that makes them sick. We have to raise animals in a way that encourages their health and then we don’t need to use antibiotics.”
Just last month, raw beef and chicken contaminated with antibiotic resistant salmonella was discovered in 36 states. Millions of pounds of meat were recalled and hundreds of people got sick.
So, we wondered how easy it would be to find antibiotic resistant bacteria if we did our own random sampling.
Turns out, very easy.
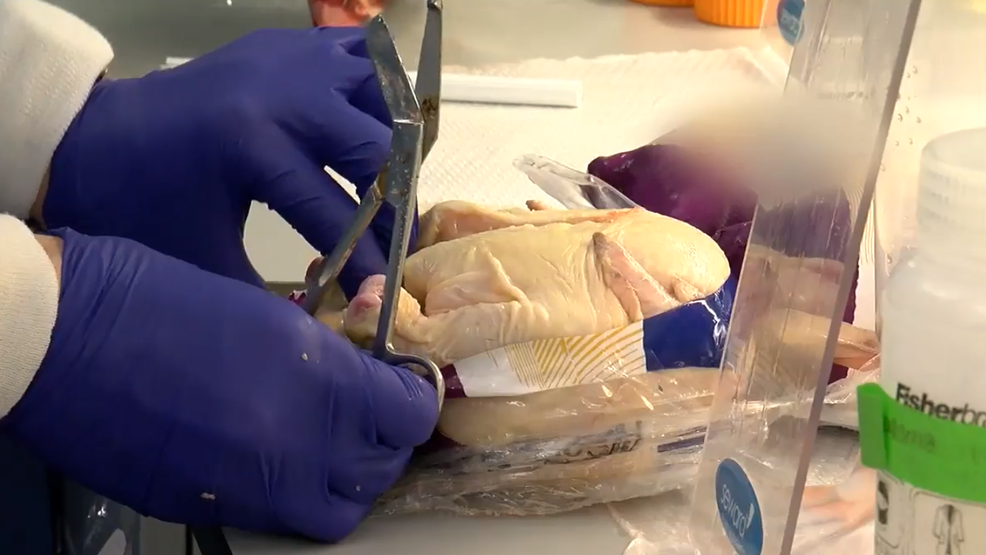
We bought two dozen samples of poultry from four major national retailers, ranging from chicken breasts and ground chicken, to ground turkey, turkey burgers and drumsticks.
In one afternoon we purchased, labeled, and packed every single package on ice and hand delivered our coolers to Dr. Price’s lab.
The testing was done in two phases.
First, Dr. Price’s lab identified the four most-common bacteria to cause foodborne illness: E coli, Salmonella, Staphylococcus, and Campylobacter.
Then, they determined if the bacteria were antibiotic resistant.
Two weeks later, the results were in: 88 percent of our samples harbored antibiotic-resistant-bacteria. And not just one type.
Combinations of E. coli, Salmonella, Campylobacter and Staphylococcus were resistant to antibiotics anywhere from two to 17 times per sample. Drugs considered to be some of the most important on the planet like Amoxicillin, Cipro and Tetracycline, were often rendered useless.
“Ninety percent, basically, of the samples that you gave us were positive for E. coli,” said Price. “We have probably animal feces in all of that meat. But it’s also an important pathogen and when we look at what E. coli was resistant to, one of the drugs it was most resistant to, or most often resistant to, was tetracycline. Which is also the drug we use most often for animal production in the United States.”
Tetracycline is considered by the World Health Organization to be one of the most important antibiotics on the planet. It, and numerous other drugs categorized as “critical” to human health failed in most of our tests against the bacteria we found on grocery store meat.
And the lab found more that we didn’t expect.
“On three of the turkey samples we found Methicillin-resistant Staphylococcus aureus or MRSA. I mean, that was a little shocking to me,” said Price. “When they get past our skin they can infect our blood. They can infect our hearts and kill us. At one point, probably still today, MRSA kills more people than HIV in the United States.”
Price says the problem with antibiotic-resistant-bacteria is that it exists everywhere in conventional meat production, making types of meat, brand names and stores irrelevant.
And the government is well-aware of the problem.
Every year the USDA tests thousands of pieces of grocery store meat for antibiotic resistant bacteria through the National Antimicrobial Resistance Monitoring System, or NARMS. The data goes largely unnoticed by the public.
“Resistance is real. Resistance is here. It’s now. We’re seeing it. It kills 23,000 Americans each year,” Dawn Undurraga told us.
Undurraga has analyzed more than 47,000 government lab tests of bacteria on supermarket meat for the Environmental Working Group. That data’s been used to identify trends and impacts on public health.
The most recent report shows 75 percent of bacteria found on grocery store meat is antibiotic resistant, including 73 percent of salmonella on ground turkey. Of pork chops the government tested, 71 percent were positive for antibiotic resistant bacteria.
Thoroughly cooking meat will kill the bacteria. But Price says the bacteria are typically spread far beyond the meat itself – from the grocery cart at the store, all the way to your kitchen.
“So, you open a package of chicken,” said Price. “You have a contaminated package to deal with, right? So, you open the trash can, you contaminated that. You’re going to go wash your hands, so you turn on a faucet. You’ve just contaminated the faucet. You’re going to pump the soap, contaminate that. You’re going to wash your hands really well. You shut off the faucet, re-contaminate your hands, go make a salad. So that’s how easy it is to spread these bacteria into the kitchen.”
There is no dispute that antibiotic resistance is complicated. Price says while four times more antibiotics are given to farm animals than humans, overprescribing in the doctor’s office is contributing to the problem.
The drugs, some of which no longer work, are all drugs medical science relies on to stop treatable infections before they become critical or even deadly.
“This is a serious threat to public health,” said Undurraga. “If we don’t do something, we could enter a post-antibiotic era where things like a scratched knee or pneumonia could kill people again.”
There’s very little regulation in conventional animal agriculture to prevent industry from overusing antibiotics, leaving it up to individual companies to make critical decisions about public health. Price says the Obama administration made significant progress on the issue – banning the practice of giving antibiotics purely to make animals grow faster, but the industry found work-arounds.
“Our lifesaving antibiotics, for years, for decades, were used just to make animals grow faster,” said Price. “But there’s still this big loophole which allows food animal producers to give animals antibiotics to prevent disease. And that’s a loophole big enough for 34 million pounds [of antibiotics to] go through. So, they raise animals in a way that makes them sick and then they justify the antibiotics.”
“We’re sending a message to the world that says this is OK,” said Price. “And that’s going to come back to bite us.”
Statement from National Chicken Council:
“More than half of the chicken meat produced in the U.S. is now produced without the use of antibiotics. Per FDA guidelines, antibiotics are only administered to treat and prevent disease in livestock, only under the prescription of a licensed veterinarian. If an antibiotic is used on the farm, federal rules require the antibiotics to have cleared the animals’ systems before they can be slaughtered. For approved antibiotics, FDA and the U.S. Department of Agriculture (USDA) have extensive monitoring and testing programs to make sure that food at the grocery store does not contain antibiotic residues.
“According to the most recent report from the FDA, Salmonella and Campylobacter prevalence in retail chicken meat samples continue to decline, and both are at their lowest levels since NARMS began testing.
“Though we’ve collectively made tremendous progress in reducing pathogens, the fact is raw chicken is not sterile, and any raw agricultural product, whether its fresh fruit, vegetables, fish, meat or poultry, is susceptible to naturally occurring bacteria that could make someone sick if improperly handled or cooked.
“We all play an important role in ensuring food safety for our families, and there are steps people can take in the home to significantly reduce any risk. For raw chicken, that means washing your hands before and after contact, not cross contaminating other surfaces, cutting boards, knives, etc. and cooking chicken to a minimum internal temperature of 165 F. Even though bacteria may be resistant to some antibiotics, it is not resistant to the proper heat from an oven or grill.”
Statement from Director of Regulatory and Scientific Affairs KatieRose McCullough, Ph.D., MPH at the North American Meat Institute:
“It’s a fundamental fact of nature that raw agricultural products like poultry contain bacteria and it’s our job to reduce those bacteria to the lowest levels possible. U.S. Department of Agriculture data show our efforts to reduce bacteria are working and Centers for Disease Control data show that foodborne illnesses in humans are also declining.
Just like humans, animals sometimes need antibiotics and they are administered under veterinary oversight to ensure that they are used appropriately. When antibiotics are given, strict withdrawal periods are followed before birds are processed into food. Used properly by expert veterinarians, antibiotics are very effective in destroying bacteria and ensuring animal health. But occasionally, some bacteria survive and become resistant to an antibiotic. The good news is that being resistant to one antibiotic doesn’t mean a germ is resistant to all antibiotics.
Meat and poultry scientists are always working to develop the best strategies possible to target and destroy bacteria that can cause illness while preserving the effectiveness of antibiotics. While no foodborne illness is acceptable, the fact is that that Americans eat billions of servings of poultry every year and more than 99.99 percent of those servings are consumed safely. The public should follow good safe handling and cooking practices and know that poultry companies are committed to providing the public with products that are as safe as we can make them.”
Source link