[ad_1]
"That turned out to be absolutely correct," said Hoyte-Badu, who was 24 when she participated in the program. "They just appreciated that someone really listens to them and is understanding and non-critical."
His leadership role was part of a new study on denominational approaches in the treatment of hypertension in the black community; the results were published Tuesday in Circulation: Cardiovascular Quality and Outcomes Journal.
The researchers found that people who received counseling about their therapeutic lifestyle and motivational interviews in a church had a greater reduction in systolic blood pressure levels than those who received health education in churches.
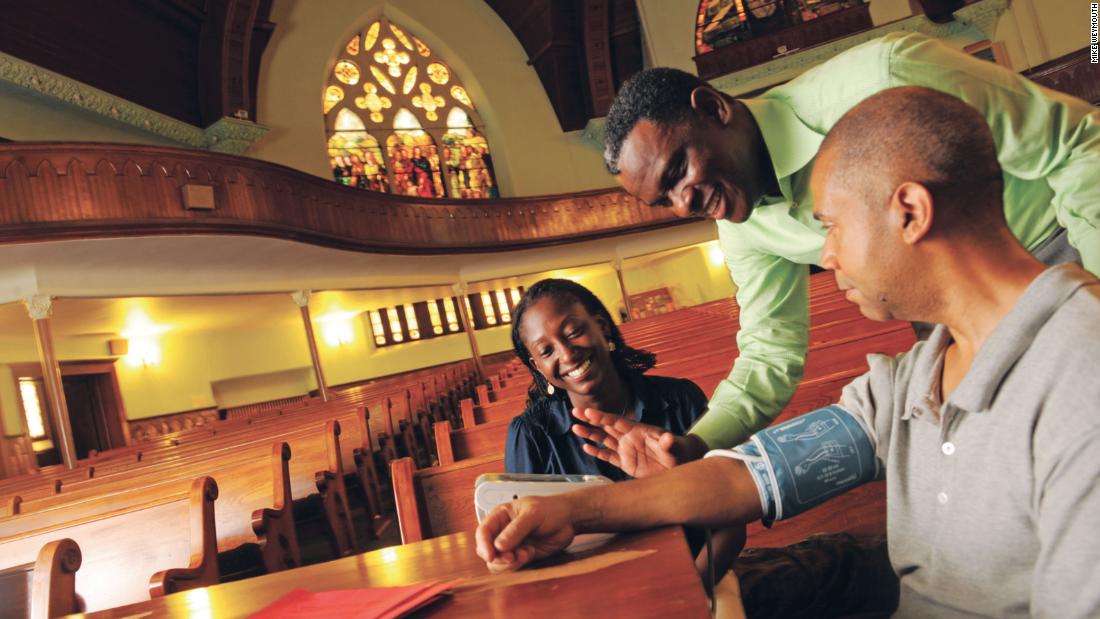
For the new study, the researchers divided 373 people from 32 churches in New York City into two groups. One of them, called the MINT-TLC group, attended 11 weekly 90-minute group sessions devoted to healthy lifestyle changes. The sessions were led by church members acting as non-professional health advisers. These were followed by three monthly phone calls to inform one of the group leaders of the weekly sessions of their progress.
The other group received a session dedicated to the lifestyle devoted to high blood pressure, also called hypertension, and ten sessions given by health experts on another topic, such as the disease. Alzheimer's or fire safety. The members of this group did not receive motive calls.
The blood pressure of both groups was measured at the beginning of the program, six months after the start of the program and nine months after the start of the program.
The church of Hoyte-Badu was one of the first to get involved in the project.
She said that she wanted to bring this project in there because of the prevalence of high blood pressure and her own experience with family members suffering from hypertension.
"I thought it would be great to work with a program that would help people with this disease reduce their high blood pressure and simply give them the skills they need to improve their overall health," she said.
In her role as a health consultant, Hoyte-Badu has been trained to lead sessions on topics such as lowering blood pressure and setting goals for improving health. She and two other counselors from her church also followed the participants in the months following the intervention.
"The program has encouraged more dialogue and collaboration, as opposed to what we give them lectures, and I think they appreciate that we are more collaborators rather than teachers," Hoyte-Badu said. "I think it created a safe environment and a supportive environment so that they could share how they came out with the challenges and feel comfortable sharing their journey by trying to do it." behavioral changes, because it's really difficult. "
Sessions were always opened with a prayer from a health advisor or participant, including scriptures related to the subject of the week, said Hoyte-Badu.
The members of her church welcomed the project and were delighted to be part of it, she said. At the end of the program, they ate a coffee-based meal and all bought a healthy dish that they had learned or had found.
She also said that the study helped fill a gap in the literature on the effectiveness of faith-based intervention projects.
"Faith-based settings tend to be sources of reliable information, so when public health can align with these sources of trust in community efforts, it strengthens disease prevention and disease promotion activities. health, "she said.
The study "supports the notion that community-based non-clinicians can be effective messengers for healthy behavioral change in blacks suffering from high blood pressure," said Ravenell, who does not discuss the issue. did not participate in the new search.
Ravenell also praised the latest study for his setting and his focus on the need to alter the lifestyle of black adults with high blood pressure, which he describes as "a cornerstone of treatment for the treatment of hypertension." 39, both underestimated and under-studied blood pressure in black populations. "
Source link


