
[ad_1]
More than one million women have undergone genetic testing on the BRCA1 and BRCA2 genes, genes in which mutations can significantly increase the risk of early breast and ovarian cancer. But for many women, the test results were ambiguous. This is because it is unclear where certain genetic variations are harmless or cause cancer.
BRCA1 was among the first cancer susceptibility genes discovered and has been studied for more than 20 years. The gene produces a protein that repairs the damage to DNA, which could lead to the formation of tumors. Since its discovery, researchers and clinicians have identified many genetic variations in BRCA1, but for most of them, we can not say they alter gene function – increasing the risk of cancer – or they are perfectly harmless.
Our research team is working in the emerging field of genomic medicine, which uses the genetic information of an individual to prescribe care. We recognized that these "variants of uncertain significance" limited the usefulness of genetic testing and the perspectives of genomic medicine. We know that the problem is likely to worsen, as the number of uncertain variants in the BRCA1 gene and other "medically activatable" genes is expected to grow exponentially as genetic tests are expanded to larger populations. whole.
In one study, we undertook to apply the CRISPR genome modification to solve the problem posed by these variants of uncertain significance. CRISPR has huge potential because technology allows researchers like us to tinker with human genes. CRISPR allows us to make very specific modifications, "modifications" to our DNA – thus, the phrase "genome editing".
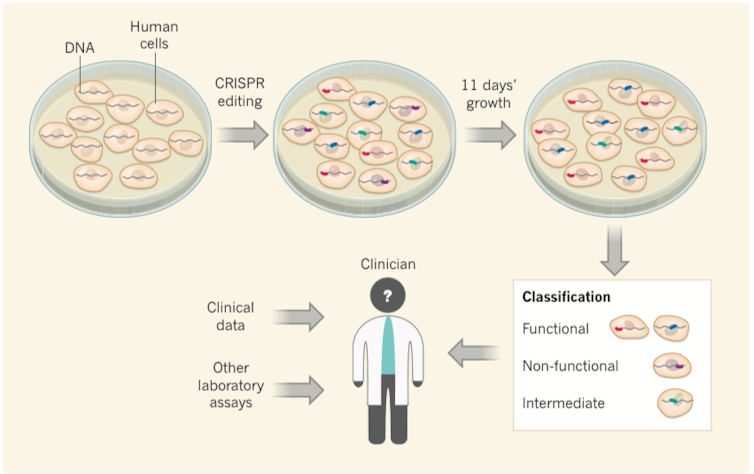
Although there are many studies that attempt to use CRISPR to treat the disease, it can also be used to introduce specific mutations into the human cells that develop in a dish, for the purpose of reducing the risk of disease. to study the effects of these mutations on the cell. whether or not they cause a dysfunction of a gene.
In our study, we used the CRISPR genome edition to deliberately design some 4,000 different variants of the BRCA1 gene in human cells, almost every possible variant in the most important regions of this gene. Importantly, the survival of the human cells we used depends on the intact function of the BRCA1 gene. As a result, cells containing mutations disrupting the function of the BRCA1 gene were unable to survive. In contrast, cells containing mutations that had no effect on the function of the BRCA1 gene were fine. Using DNA sequencing, we followed the mutations associated with cell death versus cell survival.
When we compared the mutations at the origin of cell death to variants known to increase the risk of cancer, we found that they were identical. This gave us the confidence to say that the behavior of these variants in the cells of the dish was predictive of the risk of cancer in humans.
Findlay, et al., Nature., CC BY-ND
Although scientists have used laboratory tests to test BRCA1 variants for many years, our work is different for three reasons.
First, we tested many more variants than ever before, including thousands of cases never seen before, but certainly exist in at least hundreds of human beings.
Second, historically, BRCA1 variants have been tested on genes taken "out of context," particularly by studying only the DNA sequences that encode BRCA1, rather than the surrounding sequences that regulate its expression. CRISPR allows us, for the first time, to create and test the mutations of the human genome itself.
Finally, for the hundreds of BRCA1 variants observed in patients in which we have a good idea of the increase or decrease in the risk of breast and ovarian cancer, our predictions based on our CRISPR studies are almost perfectly accurate. . That is, variants compatible with cell survival in our assay are benign in patients, while variants that impair cell survival in our assay carry a risk of cancer. This gives us confidence in our predictions for other variants that have never been observed before, but will inevitably be, especially as more and more women are screened for mutations in this gene.
Because of this strong agreement with "Gold Standard" data derived from human studies, we predict that our results can be used to provide better responses to women with variants that are difficult to interpret in BRCA1. This includes many women who are at high risk of cancer, but who would have been ignored by genetic testing. For these women, this knowledge of what their mutations mean can critically inform the medical care they receive.
Source link