[ad_1]
Private insurers across the country and Texas have engaged in the very public fight against opioid addiction, with some totally refusing coverage of OxyContin, the best-known drug related to the crisis.
But the move has sparked conflict around his wisdom, with the insurance industry defending the crackdown as a major deterrent while some members of the drug treatment and pain management communities of Houston call this an overreaction and question.
"This is a practical solution," said James Langabeer, a professor of emergency medicine at UTHealth's McGovern Medical School, who also leads the Houston Engagement Opioid Engagement System to help patients navigate the options available. treatment and recovery.
"On the one hand, it's good that the insurance industry is weighing," he says, "but I do not think we should isolate one category of opioids over another."
The concern is that those who are already addicted will not be arrested if their drug of choice becomes harder to obtain. They can simply turn to another prescription opioid or street drug, such as heroin, which can sometimes be cheaper and easier to obtain, said Mr Langabeer.
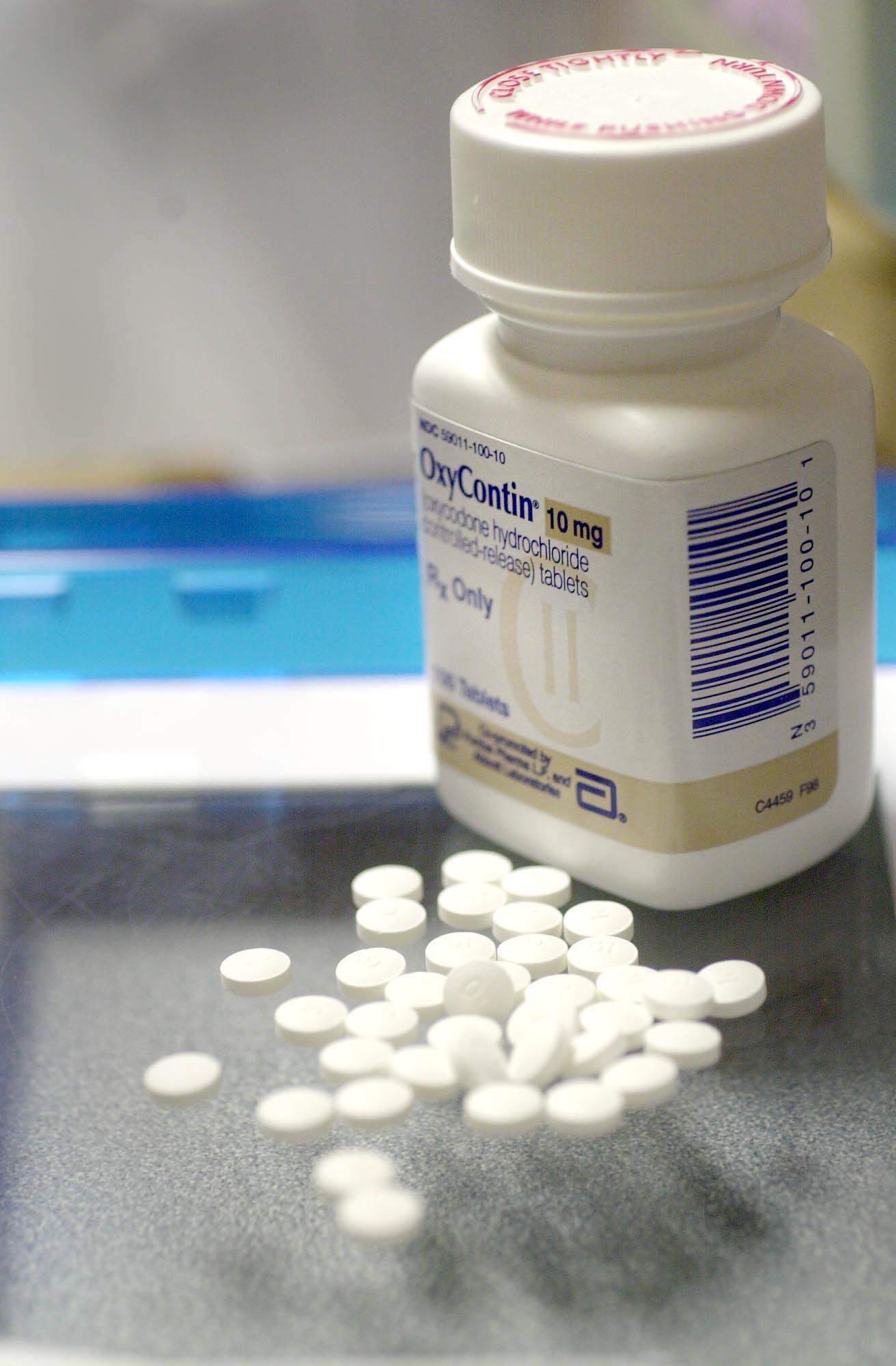
OxyContin, manufactured by Purdue Pharma, is the brand name of Oxycodone, a narcotic drug used to treat moderate to severe pain. In recent years, the drug maker has been at the heart of scandals and litigation. There are allegations that he intentionally misled physicians about the safety of the dose increase. In May, Texas sued Purdue Pharma, arguing that misleading marketing had fueled the opioid crisis.
"Trace a line"
Last week, Blue Cross and Blue Shield of Tennessee, the state's largest insurer, became the last company to announce that it will stop taking OxyContin prescriptions as of January 1, 2019. Company officials we will not continue to pay for it.
The announcement follows the national shutdown of two giants of National Insurance, Cigna and UnitedHealthcare, which together account for millions of Texas members.
Last fall, Cigna made headlines by announcing that it was abandoning OxyContin's coverage of its list of preferred medications for employer-sponsored health plans starting this year. About a million Texans have such projects, said a spokesman for Cigna.
Cigna clients who are already taking the drug for palliative care or cancer treatments will be covered by the end of 2018, the company said. After that, the insurer "will consider approving coverage for Oxycontin if a client's physician believes that OxyContin treatment is medically necessary," said a statement emailed to the Chronicle.
UnitedHealthcare has quietly stopped covering OxyContin in its employer-sponsored plans on January 1, 2017. More than 3 million Texans have these plans.
"There are equivalent and covered therapeutic alternatives that can be used for pain indications," a spokesman for UnitedHealthcare said Monday in a statement.
These include non-opioid prescriptions as well as other pain management treatments such as chiropractic services and physical therapy, said the insurer, although the alternatives are not clearly defined.
RELATED: OTC drugs offer better pain management than opioids, says new study
Florida Blue, Florida's largest insurer, also stopped covering OxyContin for its group and individual members early in 2018.
Cigna and Florida Blue will replace Oxycontin as the drug of choice with Xtampza, an oxycondone substitute that the company finds more difficult to abuse. Blue Cross and Blue Shield of Tennessee will encourage doctors to prescribe Xtmapza or Morphabond, also opioid. The insurer said that doctors can continue to write prescriptions for the drug, but that these will not be systematically covered.
OxyContin Maker responds
Purdue Pharma reacted strongly to the blanket ban, saying it had already taken steps to make the product more difficult to use by changing the formula. He also accused insurers of supporting competitors for financial gain.
"These recent decisions by insurance companies limit prescribers' options to help resolve the opioid crisis," a company spokesperson said in a statement sent by email.
"Unfortunately, these decisions seem to be more related to pharmaceutical discounts," the statement said.
Rather than banning the drug, Texas regional insurers are taking a different approach.
Blue Cross and Blue Shield of Texas announced on Monday that they would continue to cover OxyContin for its members, but that the company has put in place a series of safeguards to detect and reduce potential overuse.
The Company's appropriate opioid use program was launched on August 1 and will be phased in over eight months. As part of the program, the state's largest insurer will review the quantity and dosage of prescriptions for opioids and will check that different doctors are writing similar prescriptions for a patient, according to the insurer.
"The BCBSTX Prescription Drug List is regularly reviewed to determine which drugs are safe, effective and affordable. Updates to the list of medications – such as the removal / addition of drugs – are based on these guidelines and other changes in the pharmaceutical market, "the insurer said in a statement.
RELATED: A Houston doctor, director of the clinic of a so-called pill mill among hundreds of people accused by the force of strikes
Community Health Choice, a Houston-based health insurer, will also continue to cover OxyContin, but will limit the number of pills prescribed and will monitor multiple prescriptions directed to the same patient, as well as follow-up of doctors who appear to prescribe medications, said Dr. Karen Hill, senior vice president of medical affairs for the insurance company
She does not know if the banning of a drug can be effective in the global fight against the opioid crisis. "We think it's a narrow vision," she said.
OxyContin has been a proven benefit for some patients, including those with cancer, at the end of their life or after surgery, she said.
Dr. Brian Bruel, Associate Professor of Physical Medicine and Rehabilitation at Baylor College of Medicine, goes further. "For me, it is the insurers who practice medicine," he said.
By the numbers
Yet no one disputes the horror of the numbers.
According to the Centers for Disease Control and Prevention, the United States currently has the highest rate of overdose deaths ever recorded. In 2016, there were 42,000 drug overdose deaths involving opioid prescription pain relievers. 116 people die every day.
And while Texas has not experienced the ravages of opioids in other states, it has been reported as a "significant" increase in overdose deaths, reaching 2,831 in 2016, up from 2,588 in 2015, according to the CDC.
RELATED: Deaths related to prescription drugs in Texas are largely underestimated
Katharine Neill Harris, a drug policy fellow at the Baker Institute of Public Policy at Rice University, has mixed feelings about the insurers' entry into the fight. While, like others, she said she was happy to see the action, she wondered if it was too late to come and not the best way.
"They have a role to play and I do not think they've done enough," she said, adding, "The best way to say we're doing something is to stop covering a drug.
Although she is cautiously supportive of restricting opioids in new patients, she believes that physicians should have the discretion to recommend painkillers that they already know how to work for established patients.
What Harris would really like to see is that the insurance industry and doctors are more inclined to explore other remedies, such as long-term physical therapy for chronic pain, rather than to take a block of medication.
Source link