
[ad_1]
There are about 100 trillion cells that make up the human body. A new megascience effort will catalog and represent each of 200 cell types or more of the 80 known organs and identify the active genes in these cells.
This new effort is a follow-up to the human genome project that engulfed biology in the 1990s and early 2000s. Now scientists have come up with an exciting new challenge: to create a cellular map of the whole human body, a project called Human BioMolecular Atlas Program, or HuBMAP. The University of Florida is one of five participating tissue mapping centers. Here at the UF Center, we are responsible for mapping the thymus, lymph nodes and spleen, all key components of the immune system.

S K Chavan / Shutterstock.com
I've been studying type 1 diabetes or juvenile diabetes for almost 35 years and, along with my other colleagues at the UF Diabetes Institute, I've been trying to find a way to prevent and cure disease. This has been a challenge until recently because we did not know what caused type 1 diabetes.
Our goal as a tissue mapping center is to identify the unique types of cells, the proteins that they produce and the activated genes, and build a three-dimensional virtual model of each organ. This map will inform research of many diseases, including type 1 diabetes.
Why understanding the causes of type 1 diabetes is important
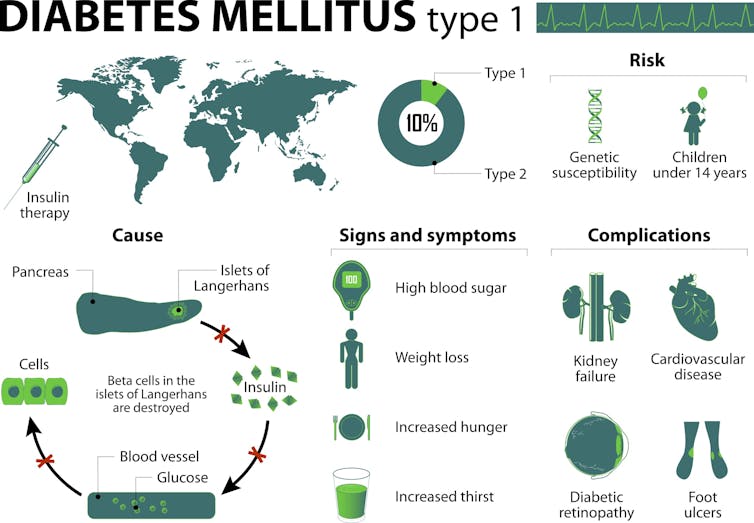
We know that type 1 diabetes is an "autoimmune disease". In type 1 diabetes, immune cells called "T cells" are thought to destroy the pancreatic beta cells responsible for producing insulin. in our blood.
A little over ten years ago, frustrated by the inability to prevent and cure the disease, I launched an initiative to collect the human pancreas from organ donors with diabetes type 1, as well as those who did not suffer from it. This last group was collected to understand the "normal" healthy pancreas. To date, we have collected the pancreas of more than 500 people. We distributed these handkerchiefs to some 230 projects in 21 countries around the world. The results of this effort have led to new discoveries that have rewritten our understanding of how this disease develops.
Designua / Shuterstock.com
Patients diagnosed with type 1 diabetes, approximately 25,000 per year in the United States alone, are dependent on daily insulin injections to survive and present a high risk of long-term medical complications: blindness, kidney failure, amputations and cardiovascular diseases. Today, an estimated 1.25 million people in the United States live with this disorder.
As troubling as these complications are in people with the disease, the many everyday lifestyle factors that need to be controlled or addressed to control the disease may be even more discouraging: carbohydrate monitoring, estimating exercise, blood glucose evaluation and insulin administration. to avoid high and low blood sugar levels. These are just some of the daily difficulties associated with the disease.
For these reasons, the goal of our collective research efforts at the UF Diabetes Institute has always been to understand the causes of this disease. Knowing this, we can predict who is at risk, identify ways to prevent disease progression and develop a cure.
Why study these organs?
Type 1 diabetes is only one of 80 known autoimmune diseases whose immune system turns against itself for unknown reasons. Beyond autoimmunity, immune responses are also a key element of health in terms of fighting cancer and infectious diseases. From our experience in the study of the pancreas and type 1 diabetes, we see great progress in understanding the role of immunity in each of these contexts through mapping. This will dive deep into the functioning of the immune system.
In a healthy individual, T cells become active only when they respond to infection or cancer cells. But in people predisposed to autoimmune diseases, some T cells can be activated erroneously by "auto" proteins, which leads them to destroy healthy tissue.
In other circumstances, such as cancer or infectious diseases, the immune system fails to provide a sufficiently robust response to be effective. Or, the cells of the immune system proliferate uncontrollably, resulting in cancers of the blood and lymphatic vessels such as lymphoma and leukemia. This is why the thymus, spleen and lymph nodes are of interest to those who are studying the healthy human immune system. Researchers must understand the healthy foundations of all these organs in order to recognize dysfunctions and changes, leading to autoimmune diseases, cancer and infectious diseases. In other words, we must first understand what constitutes the normal lymphatic system throughout human life.
Why define normal is important
You might be wondering where exactly we are getting these normal cells. As we have done in the past 11 years, we will obtain transplanted quality human tissue from deceased organ donor organs, after a family member or an executor legal authority has given informed consent. At a time of mourning, these valuable anatomical gifts, which in the case of the spleen, thymus and lymph nodes, are not usable for transplantation procedures, constitute an inimitable resource for scientific research and discovery.
Only tissues considered "normal" – unaffected by known or observable pathologies – will be included in these initial studies. We will collect donor tissue from infants to adults under 70 years of age. We hope this will provide insights into how age changes the type and health of all cells in each organ.
A multidisciplinary team including cellular and molecular biologists, hematopathologists who are studying clinical lymphatic specimens, biomedical engineers, immunologists and many others will collaborate on the HuBMAP program. Indeed, UF's tissue mapping center will work closely with a worldwide network of experts in advanced microscopy and data collection.
We are establishing an imaging pipeline to detect dozens of protein and RNA molecules that characterize nerves, blood vessels, supporting tissues known as stroma, and immune cells derived from slices of fabric.
In the first two years of HuBMAP, we plan to map the spleen, thymus and lymph nodes in 11 organ donors.
We expect that the data obtained will reveal new cell types, molecular and cellular structures, cell-cell interactions, and their functional implications in human anatomy and physiology. Therefore, the three-dimensional high resolution human biomolecular atlas program should facilitate discovery.
By the end of my fifties, the number of colleagues, friends and family members affected by the disease is increasing every year. I also recently became grandfather. I would like to think that what we propose to do will have a dramatic impact on human health for present and future generations. It would be a legacy gift.
Source link