
[ad_1]
The 2017-2018 flu season was historically severe. Public health officials estimate that 900,000 Americans have been hospitalized and 80,000 died of flu and its complications. For comparison, the previous worst season of the past decade, 2010-2011, saw 56,000 deaths. In a typical season, 30,000 Americans die.
So why was the 2017-2018 season such a bad year for flu? There were two big factors.
First, one of the circulating strains of the influenza virus, A (H3N2), is particularly virulent, and vaccines targeting it are less effective than other strains. In addition, most of the vaccine has been mismatched to the circulating A (H3N2) subtype.
These problems reflect the special biology of the influenza virus and the methods by which vaccines are produced.
Flu virus is a quick change artist
Influenza is not a single, static virus. There are three species – A, B and C – that can infect people. A is the most serious and is rare, producing only mild symptoms. Flu is further divided into various subtypes and strains, based on the viral properties.
Timonina / Shutterstock.com
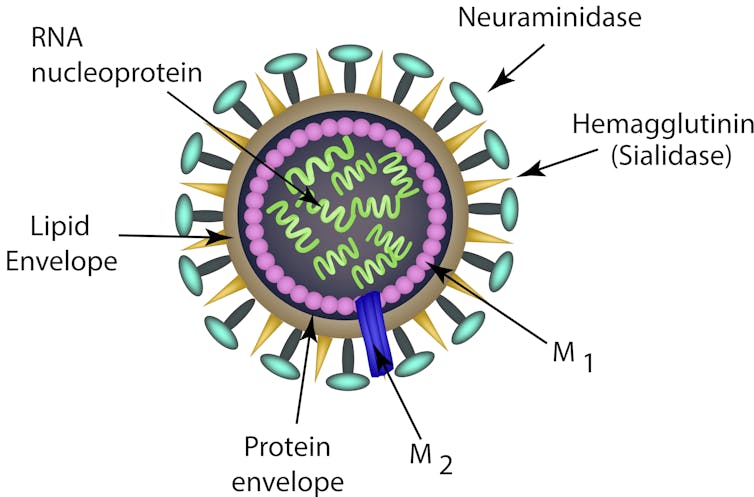
Viral genome, which, in the influenza virus, consists of RNA divided into eight separate segments. The influenza virus is enveloped by a membrane layer derived from the host cell. These haemagglutinin (HA) and neuraminidase (NA) proteins are both effective for infection.
Your immune system reacts first to these two proteins. Their properties determine the H and N designations of various viral strains – for instance, the H1N1 "swine flu" that swept the globe in 2009.
Both HA and NA are changing. The process that copies the viral RNA genome is inherently sloppy, plus these two proteins are under strong pressure to evolve so they can evade attack by the immune system. This evolution of HA and NA proteins, called antigenic drift, prevents people from developing lasting immunity to the virus. Although the immune system may be prepared to shut down strains, even minor changes may be necessary. Thus we have seasonal flu outbreaks.
In addition, various subtypes of influenza A infect animals, the most important of which, for humans, are domestic birds and pigs. If an animal is infected with two different subtypes, the segments of their genomes can be scrambled together. Any resulting virus may have new properties, to which humans may have little or no immune defense. This process, called antigenic shift, is responsible for the major pandemics that have swept the world in the last century.
Forecasting flu, producing vaccine
Against this background of antigenic changes, every year in the World Health Organization, which are likely to be affected by these viruses, and vaccines are formulated based on this information.
In 2017-2018 the vaccine was directed against specific subtypes of A (H1N1), A (H3N2) and B. The Centers for Disease Control and Prevention estimates that this vaccine was 40 percent effective in preventing influenza overall. Aim, significantly, it was only 25 percent effective against the dangerous A (H3N2) strain. This mismatch is most likely the most vaccines are produced.
The common way of producing influenza vaccine starts with growing the virus in fertilized chicken eggs. After several days, the viruses are harvested, purified and inactivated, leaving the surface proteins, HA and NA intact. But, when the virus is grown in eggs, it can grow more easily and become more common.
When people receive vaccines produced by these egg-adapted viruses, their immune systems can be affected by HA proteins and proteins. Thus, the virus used to produce much of the circulatory system in the population of the circulatory system.

AP Photo
Small improvements and a universal vaccine
Scientists are on the hunt for a better way to protect the world's population from influenza.
Two new vaccines that are not currently available. One, a vaccine made from viruses grown in mammalian cells, was only 20 percent more effective against A (H3N2) than egg-produced vaccine. The other, a "recombinant" vaccine of the HA proteins, is produced in insect cells, and its effectiveness is still being evaluated.
The ideal solution is a "universal" vaccine that would protect against all viruses, no matter how strains mutate and evolve. One effort relates to the fact that the protein is "stalk" is less variable than the "head" that interacts with the host cell surface; vaccines made from a cocktail of HA protein "stalks" have proved disappointing so far. M1 and NP, which are much less variable than surface-exposed proteins, are in clinical trials, and are other vaccines made up of a proprietary mixture of parts of viral proteins. These vaccines are designed to stimulate the "memory" immune cells that persist after an infection, possibly providing lasting immunity.

AP Photo / Jeff Chiu
Will the 2018-2019 flu season be bad?
Based in the United States, the World Health Organization recommends changing the A (H3, N2) subtype in the vaccine to one that better matches last year's circulating A (H3, N2). They also recommended changing the subtype to one that appeared in the US late in the 2017-2018 season. The WHO expected that the circulating A (H1N1) subtype will be the same as last year and so no change was necessary on that front. So, the same strains will be more likely to be circulating, epidemiologists expect the vaccines to provide better protection.
The CDC recommends that everyone 6 months and older get a shot every year, but, typically, fewer than half of Americans do so. Flu and its complications can be life-threatening, particularly for the young, the old and the otherwise debilitated. Most years the vaccine is well matched to the circulating virus strain, and even a poorly matched vaccine offers protection. Plus, wide-spread vaccination stops the virus from spreading and protects the vulnerable.
The first flu death of the 2018-2019 season has already occurred – a healthy but unvaccinated child died in Florida – affirming the importance of getting the flu shot.
Source link