[ad_1]
Fenofibrate is an oral drug approved by the FDA. The results were published on Research Square and are currently under peer review.
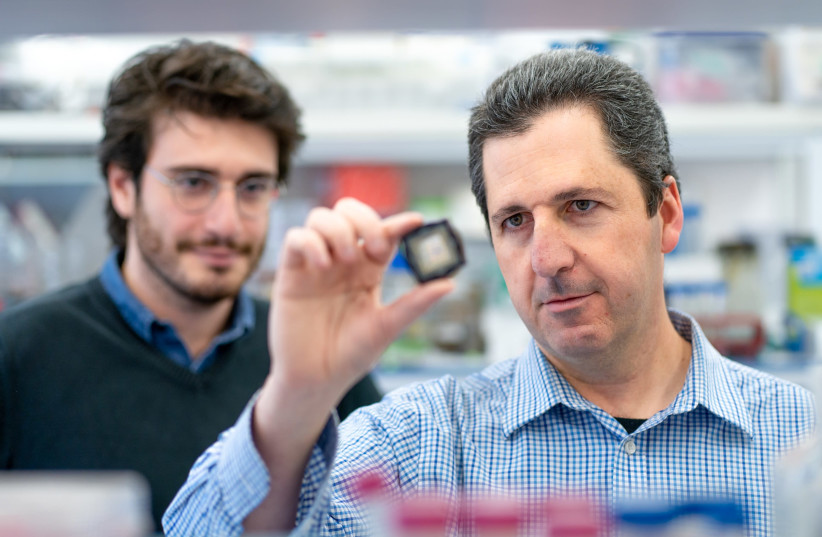
Specifically, the team led by Professor Yaakov Nahmias of HU conducted the study at Israel’s Barzilai Medical Center in coordination with the head of the hospital’s infectious disease unit, Professor Shlomo Maayan, and with the support from Abbott Laboratories.
cnxps.cmd.push (function () {cnxps ({playerId: ’36af7c51-0caf-4741-9824-2c941fc6c17b’}). render (‘4c4d856e0e6f4e3d808bbc1715e132f6’);});
if (window.location.pathname.indexOf (“656089”)! = -1) {document.getElementsByClassName (“divConnatix”)[0].style.display = “none”;} else if (window.location.pathname.indexOf (“/ israel-news /”)! = -1) {document.getElementsByClassName (“divConnatix”)[0].style.display = “none”; var script = document.createElement (‘script’); script.src = “https://player.anyclip.com/anyclip-widget/lre-widget/prod/v1/src/lre.js”; script.setAttribute (‘pubname’, ‘jpostcom’); script.setAttribute (‘widgetname’, ‘0011r00001lcD1i_12258’); document.getElementsByClassName (‘divAnyClip’)[0].appendChild (script);}
The 15 patients treated all suffered from pneumonia and required oxygen support. They were also older with multiple comorbidities, ranging from diabetes and obesity to high blood pressure.
In addition to standard care, patients received 145 mg / day of fenofibrate for 10 days.
“The results have been spectacular,” Nahmias told The Jerusalem Post. “Progressive inflammation markers, which are the hallmark of deterioration of COVID-19, fell within 48 hours of treatment. In addition, 14 of the 15 severe patients did not require oxygen within a week of treatment.
The 15th patient was deprived of oxygen within 10 days.
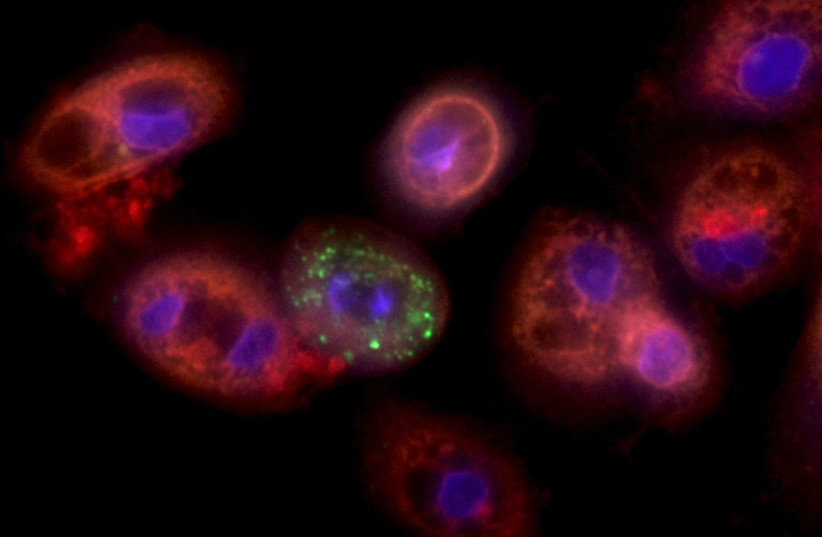 Lung cells infected with the coronavirus (credit: YAAKOV NAHMIAS)
Lung cells infected with the coronavirus (credit: YAAKOV NAHMIAS)He said that looking at data from other similar severe patients, on average, less than 30% of them are withdrawn from oxygen support in a week. In other words, fenofibrate could dramatically shorten the treatment time for severe COVID patients.
“We know that these type of patients deteriorate very quickly, develop a cytokine storm in five to seven days and that it can take weeks to treat them and get them better,” Nahmias said. “We gave these patients fenofibrate and the study shows the inflammation went down incredibly quickly. They didn’t seem to be developing a cytokine storm at all. “
Usually, patients who do not need oxygen can be treated at home. Moreover, despite the high number of deaths from COVID in Israel and abroad, the majority of critically ill patients survive.
All patients completed home treatment 10 days after discharge and, according to Maayan, “no drug-related adverse events” were reported.
Fenofibrate was approved by the FDA in 1975 for long term use and is considered safe. Plus, it’s an inexpensive pill, Nahmias said. It costs less than $ 1.50 per day, which means the total treatment per patient was around $ 15.
Nahmias has been studying the use of fenofibrate to treat COVID-19 almost since the start of the pandemic. He first conducted a preclinical trial and then a multicentre retrospective study, both of which supported the drug’s effectiveness.
“Viruses are parasites,” Nahmias explained. “They cannot replicate on their own. They must enter a human cell and hijack their machinery to replicate. “
Working with collaborators in the United States, Nahmias demonstrated that the coronavirus inhibits the burning of fat in lung cells, which results in the accumulation of large amounts of fat inside lung cells – a condition the virus can contain. needs to reproduce. Fenofibrate, he hoped, would reverse this effect and eliminate replication of the virus.
Today, he is participating in a series of Phase III studies underway in South America, the United States and Israel. These studies are placebo-controlled and double-blind.
Nahmias said his team struggled to enroll patients in the study before the Delta variant started, but efforts are now moving faster. He hopes that the results can be available within the next two months.
In the meantime, the drug is available and doctors may decide to administer it based on the available data.
“There is no quick fix,” he said, “but fenofibrate is much safer than other drugs on offer to date, and its mechanism of action makes it less likely to be specific. to a variant. “
[ad_2]
Source link