[ad_1]
Press release
Monday, June 10, 2019
An NIH-funded study shows that immunotherapy slows the progression of 2 years or more to clinical illness.
A treatment affecting the immune system has actually slowed the progression of type 1 diabetes in high-risk people, according to findings from research funded by the National Institutes of Health. This study is the first to show that clinical-type diabetes can be delayed for two years or more in high-risk individuals. These results were published online in The New England Medical Journal and presented at the scientific sessions of the American Diabetes Association in San Francisco.
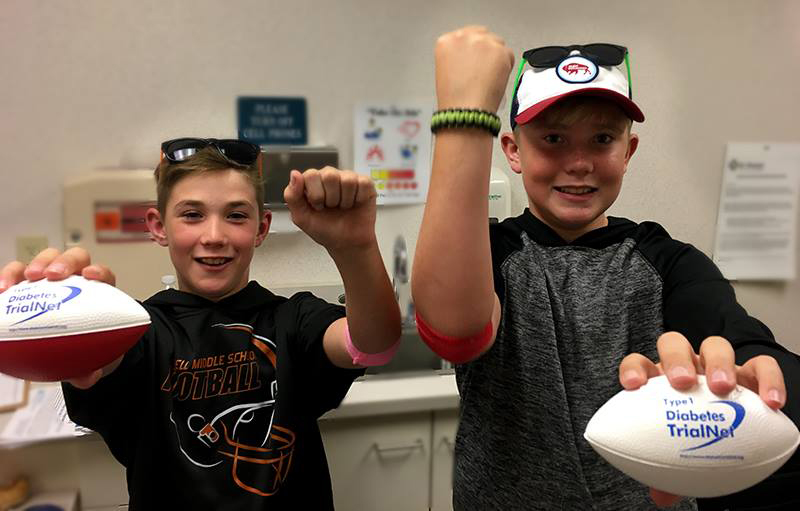
The study, involving treatment with an anti-CD3 monoclonal antibody (teplizumab), was conducted by Diabetes Type 1: TrialNet, an international collaboration to discover ways to delay or prevent type 1 diabetes. The researchers recruited 76 participants aged 8 to 49, related to people with type 1 diabetes, with at least two types of autoantibodies related to diabetes (proteins made by the immune system) and with abnormal tolerance glucose (sugar).
Participants were randomly assigned to either the treatment group, who received teplizumab for 14 days, or the control group, who received a placebo. All participants were regularly tested for glucose tolerance until the end of the study or until they developed clinical type 1 diabetes – according to the first eventuality.
During the trial, 72% of the control group developed clinical diabetes compared to only 43% of the teplizumab group. The median delay for control group members to develop clinical diabetes was just over 24 months, while those who had developed clinical diabetes in the treatment group had a median time to 48 months before moving on to the diagnosis.
"The difference in results was striking. This discovery is the first evidence that early preventative treatment can delay clinical type 1 diabetes, "said Lisa Spain, Ph.D., a project scientist at the National Institute of Diabetes, Digestive and Kidney Diseases ( NIDDK) of NIH. , sponsor of TrialNet. "The findings have important implications for people, especially young people, who have parents with the disease, as these people may be at high risk and benefit from early screening and early treatment. "
Type 1 diabetes develops when immune system T cells mistakenly destroy the body's own insulin-producing beta cells. Insulin is needed to convert glucose into energy. Teplizumab targets T cells to reduce beta cell destruction.
"Previous NIH-funded clinical research has shown that teplizumab effectively slows beta cell loss in people with recent clinical type 1 diabetes, but that the drug has never been tested in the past. people without clinical illness, "said Kevan C. Herold. , MD, from Yale University, lead author of the study. "We wanted to see if early intervention would benefit people at high risk but not yet having the symptoms of type 1 diabetes."
The effects of the drug were greatest in the first year after administration, when 41% of participants developed clinical diabetes, mainly in the placebo group. Many factors, including age, may have contributed to teplizumab's ability to delay clinical infection, as at-risk children and adolescents are known to progress more rapidly than adults to type 1. A faster progression of type 1 diabetes is associated with a very active immune system, which may explain the impact of immune-modulating drugs such as teplizumab.
Other data collected during the test may help researchers understand why some people have responded to the treatment. Participants who responded to teplizumab tended to have certain autoantibodies and other immune system characteristics. The research team also warned that the study had limitations, particularly because of the small number of participants, the lack of ethnic diversity and that all participants were parents of people with HIV / AIDS. Type 1 diabetes, which could limit the translation capacity of the study at large.
"While the results are encouraging, additional research is needed to address the limitations of the trial, as well as to understand the mechanisms of action, the long-term effectiveness, and the safety of the trial. treatment, "said Dr. Spain.
"This essay shows how decades of research into the biology of type 1 diabetes can lead to promising treatments that have a real impact on people's lives. We are very excited to see the next steps in this research, "said Dr. Griffin P. Rodgers, Director of NIDDK. "The dedicated researchers, volunteers and families involved in this program make such discoveries possible."
TrialNet offers initial screening for parents of people with type 1 diabetes, as well as follow-up testing and participation in clinical trials for people at increased risk of developing clinical disease, all for free. For more information, visit www.trialnet.org.
TrialNet (NCT00097292) is funded by the NIH, primarily through the Special Regulatory Funding Program for Type 1 Diabetes. JDRF and the American Diabetes Association provide additional support. MacroGenics / Provention Bio donated the drugs to the study and provided funds for additional monitoring of the site.
NIDDK, part of the NIH, conducts and supports basic and clinical research and research training on some of the most common, serious and disabling conditions affecting Americans. The research areas of the Institute include diabetes and other endocrine and metabolic diseases; digestive diseases, nutrition and obesity; and renal, urological and hematological diseases. For more information, visit www.niddk.nih.gov.
About the National Institutes of Health (NIH):
The NIH, the country's medical research agency, has 27 institutes and centers and is part of the US Department of Health and Human Services. NIH is the lead federal agency that leads and supports basic, clinical and translational medical research. She studies causes, treatments and cures for common and rare diseases. For more information on NIH and its programs, visit www.nih.gov.
NIH … transforming discovery into health®
[ad_2]
Source link