[ad_1]
UCSF's Benioff Children's Hospital successfully treated a one-month-old infant with rare childhood leukemia using approved targeted therapy for adults with inoperable liver cancer and advanced renal cell carcinoma .
Sorafenib chosen after pathologists identified a single mutation as two genes fused together rather than on separate chromosomes – according to a case study published in the journal Leukemia September 11, 2019.

The patient, a young child in full swing, embodies a growing change in the treatment of cancer: the genes that fuel cancer, rather than the type of cancer itself, can determine the optimal treatment, according to researchers, led by lead author Elliot Stieglitz, MD, medical scientist. within the pediatric hematology / oncology division of the UCSF and the Helen Diller Family Cancer Treatment Center.
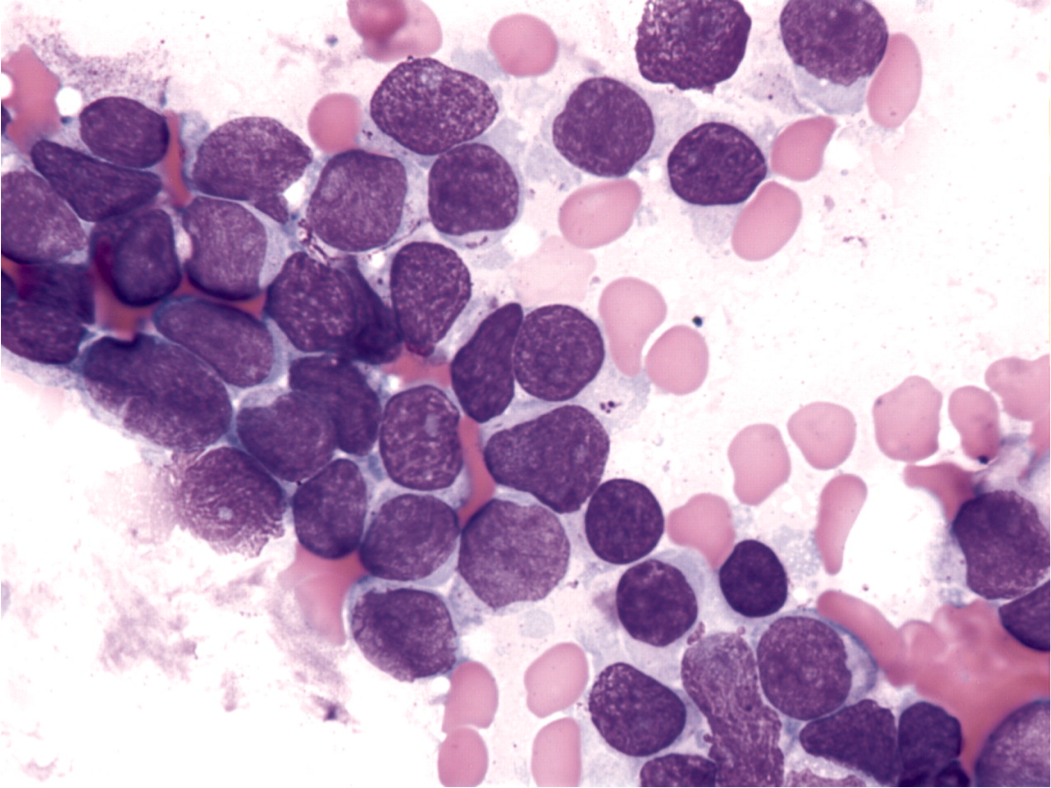
The authors report that the infant exhibited the hallmarks of leukemia, including enlarged liver and spleen, and an increase in the number of white blood cells.
The child was thought to be suffering from JMML, or juvenile myelomonocytic leukemia, a type of aggressive blood cancer most commonly affecting infants and young children, affecting about 1.2 children per million per year. JMML is treated with a stem cell transplant, in which intense chemotherapy is administered to remove JMML cells, followed by a stem cell transplant from a closely related donor in the recipient's bone marrow, where they produce blood cells. healthy. However, up to 50% of JMML patients relapse after transplantation.
Rescue treatment is broken down when the condition of the infant is declined
Chemotherapy was initiated to reduce the burden of the disease before the stem cell transplant, said Stieglitz. "Unfortunately, the patient did not respond to chemotherapy and his symptoms worsened. Stem cell transplantation was no longer an option. "
Faced with reduced options, the Stieglitz team has made a molecular profile of the child's cancer cells, hoping that the mutations can be identified and associated with targeted therapies. They used both UCSF 500, a panel of cancer genes that sequence the DNA of a patient's cancer cells and compare them to normal tissue, as well as a second tool that analyzes RNA, which offers a measure of more sensitive gene expression and can identify new features, including fusion. the genes. None of the mutations associated with JMML were found. However, pathologists were surprised to discover a mutation known as FLT3 fusion – something that had never been reported before in a malignant tumor in children, the authors said.

"We know that mergers are more likely to respond to targeted therapies than other types of mutations," said Mignon Loh., MD, co-author and chairholder in pediatric molecular oncology, who has been involved in patient care. "Sorafenib, which was developed at UCSF, is a type of targeted therapy called a kinase inhibitor that blocks the action of an abnormal protein that induces the multiplication of cancer cells."
After two weeks of treatment with sorafenib, the patient's white blood cell count plummeted to normal. After 10 weeks of treatment, the infant was fit enough to undergo a stem cell transplant. Sorafenib was stopped after almost two years. The patient remains in remission months later.
"The patient's history reveals that the single-treatment approach is not working well for all children with JMML," Stieglitz said. "The JMML course is very variable. In rare cases, children spontaneously enter remission with minimal treatment, while half of all patients suffer from a very aggressive form of the disease that does not respond to stem cell transplantation.
Most JMML patients present genes that hyperactivate the Ras pathway, Stieglitz said, referring to a protein chain in the cell that communicates a signal from a receptor to the nucleus DNA.
"Recently, it was reported that JMML patients did not have these Ras mutations, but had similar fusions to those of our patient," he said. "We recommend that all patients without Ras mutations undergo RNA sequencing to identify any fusion that could be treated with targeted therapies."
Co-authors: The first author is Alexander Chao from the Department of Pediatrics of UCSF. Co-authors are Julia Meyer, PhD, Alex G. Lee, PhD, Anna Hecht, MD, Theodore Tarver, Jessica Van Ziffle, PhD, Ashley Koegel, MD, Carla Golden, MD, Benjamin Braun, MD, PhD, and E. Alejandro. Sweet-Cordero, MD, Catherine C. Smith, MD, Christopher Dvorak, MD, and Cute Loh, MD, all of the UCSF.
Funding: The study was funded by the National Cancer Institute, the National Cancer Institute, the Alex Lemonade Stand Center Program, the Frank A. Campini Foundation and the Damon Runyon-Richard Lumsden Foundation.
Disclosures: Smith has received research funding from FujiFilm and Astellas Pharma; Chao received a fee from Bio-Rad. There are no more conflicts of interest.
The University of California San Francisco (UCSF) focuses exclusively on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, advanced science education life and health professions and the excellence of patient care. UCSF Health, UCSF's primary academic medical center, is home to leading specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.
[ad_2]
Source link