[ad_1]
Immunotherapy has been a boon for people with serious cancers. Science has been so transformative that three pioneering researchers won the Nobel Prize last year for their discoveries on the underlying immunological mechanisms that make immunotherapy drugs possible. Although these interventions have been so successful, there is still a segment of the population that is resistant to drugs and their beneficial effects, and unfortunately scientists have struggled to understand why. However, researchers at the Dana-Farber Cancer Institute, in collaboration with researchers at the Broad Institute at MIT and Harvard, have discovered that a metabolic imbalance in some cancer patients after treatment with a checkpoint inhibitor drug, nivolumab , is associated with resistance to resistance. the agent of immunotherapy and shorter survival.
The results of the new study have been published recently in Nature Communications through an article entitled "Metabolomic Adaptations and Correlates of Survival at Immune Control Point Blocking".
The chemical change, which researchers say reflects a "mechanism of adaptive resistance" of cancer cells or the immune system in response to treatment with nivolumab, an anti-PD-1 drug, has been associated with poorer survival among patients with advanced melanoma and kidney cancer. The greater the change, the conversion of the amino acid tryptophan into a metabolite called kynurenine, is important, the greater the impact on survival is important.
"The main message is that metabolic adaptations in cancer immunotherapy may be relevant after an immune checkpoint blockage," explained the study's lead investigator, Toni Choueiri, MD, director of the Center. of Lank Genitourinary Oncology from Dana-Farber Cancer Institute and Professor of Medicine at Harvard Medical School.
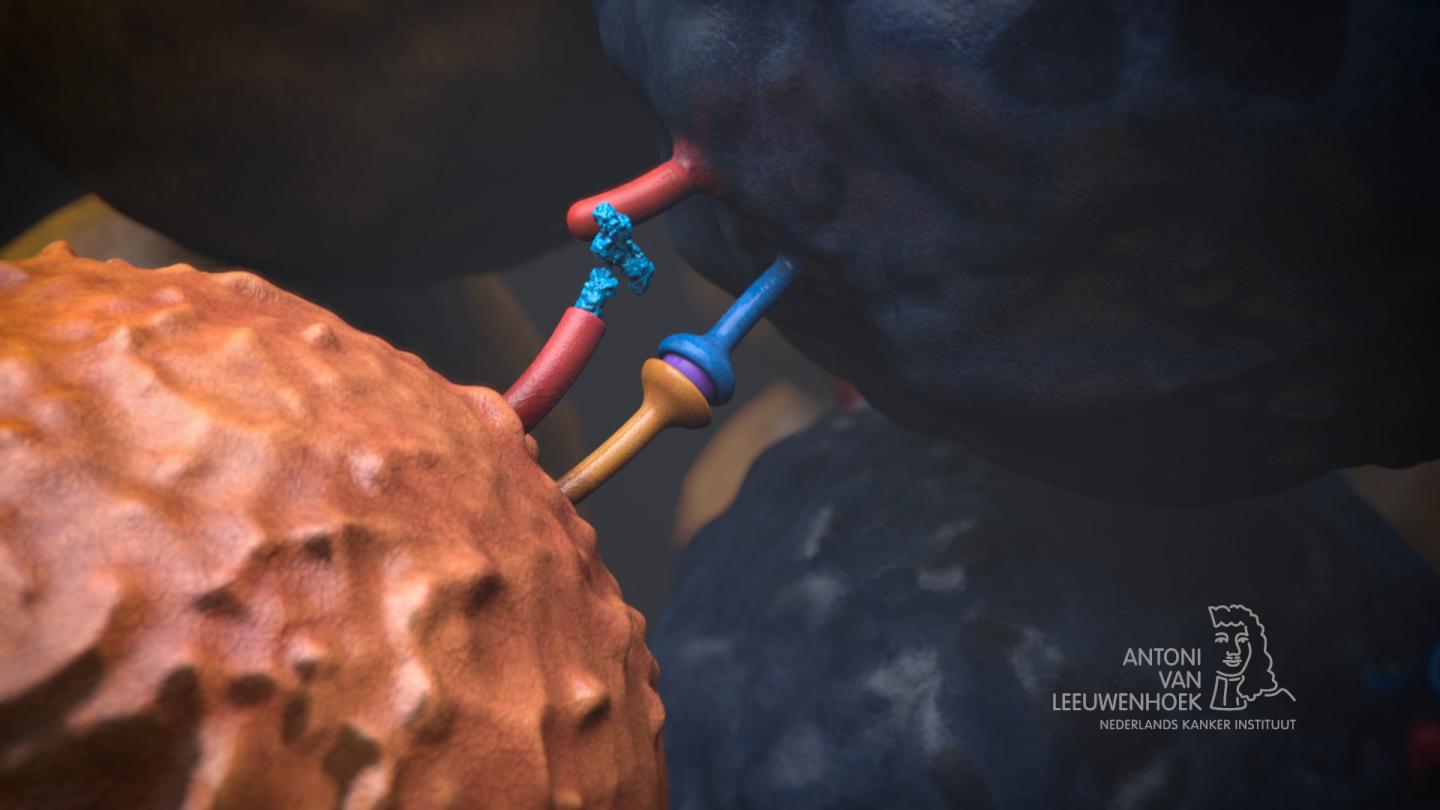
Checkpoint blockers such as nivolumab are drugs that release the molecular brakes of the immune response that cancer often uses to escape the attacks of immune T cells. Such a molecular brake is known as PD-1. In some patients and some types of cancer, the drugs have been shown to be very effective in triggering T cell attack on tumors, but overall the drugs only help a minority of patients.
"One of the most important questions in oncology is who responds and who does not respond to modern PD-1 inhibitors," said Choueiri.
Scientists have studied samples of cancer tissue to look for factors that may be associated with the greater or lesser effect of checkpoint inhibitors: among them are the number of cancer-related mutations detected in the tumor's DNA, as well as other genetic "signatures" associated with the response. checkpoint blockers. The metabolic impairment discovered by scientists in the current study could be measured in the blood – a significant advantage over tissue tests.
"It's an attractive option for identifying biomarkers of metabolic changes" related to treatment with checkpoint blockers, said Marios Giannakis, assistant investigator of the study, medical doctor, assistant professor of medicine at the Dana-Farber and Harvard Medical School. "We know that metabolism is important for immunity and that kynurenine [the chemical found to be elevated in a majority of the patients treated with nivolumab] is known to be immunosuppressive. "
In this study, researchers analyzed blood samples from three independent immunotherapy trials and measured changes in metabolites. [chemicals involved in metabolic reactions] before the start of treatment and several times during treatment. In patients with melanoma, 78% experienced an increase in tryptophan conversion to kynurenine and 26.5% experienced increases greater than 50% by the fourth week of treatment. In patients with kidney cancer, treatment with nivolumab has also been associated with an increase in kynurenine.
"In order to study metabolic alterations in response to immune checkpoint blockade, we have detailed serum metabolites in patients with advanced melanoma and renal cell carcinoma treated with nivolumab, an antibody against the death protein." programmed cell 1 (PD1) ", write the authors. "We identify the serum kynurenine / tryptophan ratio as a mechanism of adaptive resistance associated with poorer overall survival. This argues for patient stratification and metabolic monitoring as part of clinical trials of immunotherapy, including those associating PD1 blockade with inhibitors. indoline amine 2,3-dioxygenase / tryptophan 2,3-cancrdioxygenase (IDO / TDO). "
The analysis showed that patients with melanoma and kidney cancer with high levels of tryptophan conversion to nivolumab kynurenine had poorer survival. 15.7 months, while patients with a decrease in this ratio had a median survival time greater than 39 months whereas the respective number of patients with kidney cancer was 16.7 versus 31.3 month.
It is not clear how a PD-1 control point blocker was converted to tryptophan in kynurenine. However, an enzyme called IDO, implicated in many forms of cancer, plays a major role in the synthesis of kynurenine from tryptophan. The Dana-Farber researchers noted that a randomized clinical trial in which patients with advanced melanoma were treated only with IDO inhibitors did not give positive results. However, this study did not examine the kynurenine levels of these patients. The researchers said their findings suggest that the combination of control point blockers with IDO inhibitors could "benefit a select group of patients with kynurenine pathway activation triggered by inhibition of control".
[ad_2]
Source link