[ad_1]
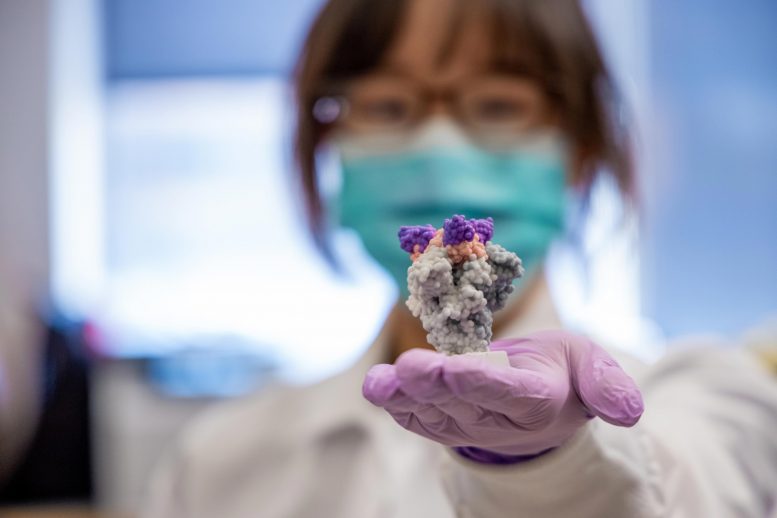
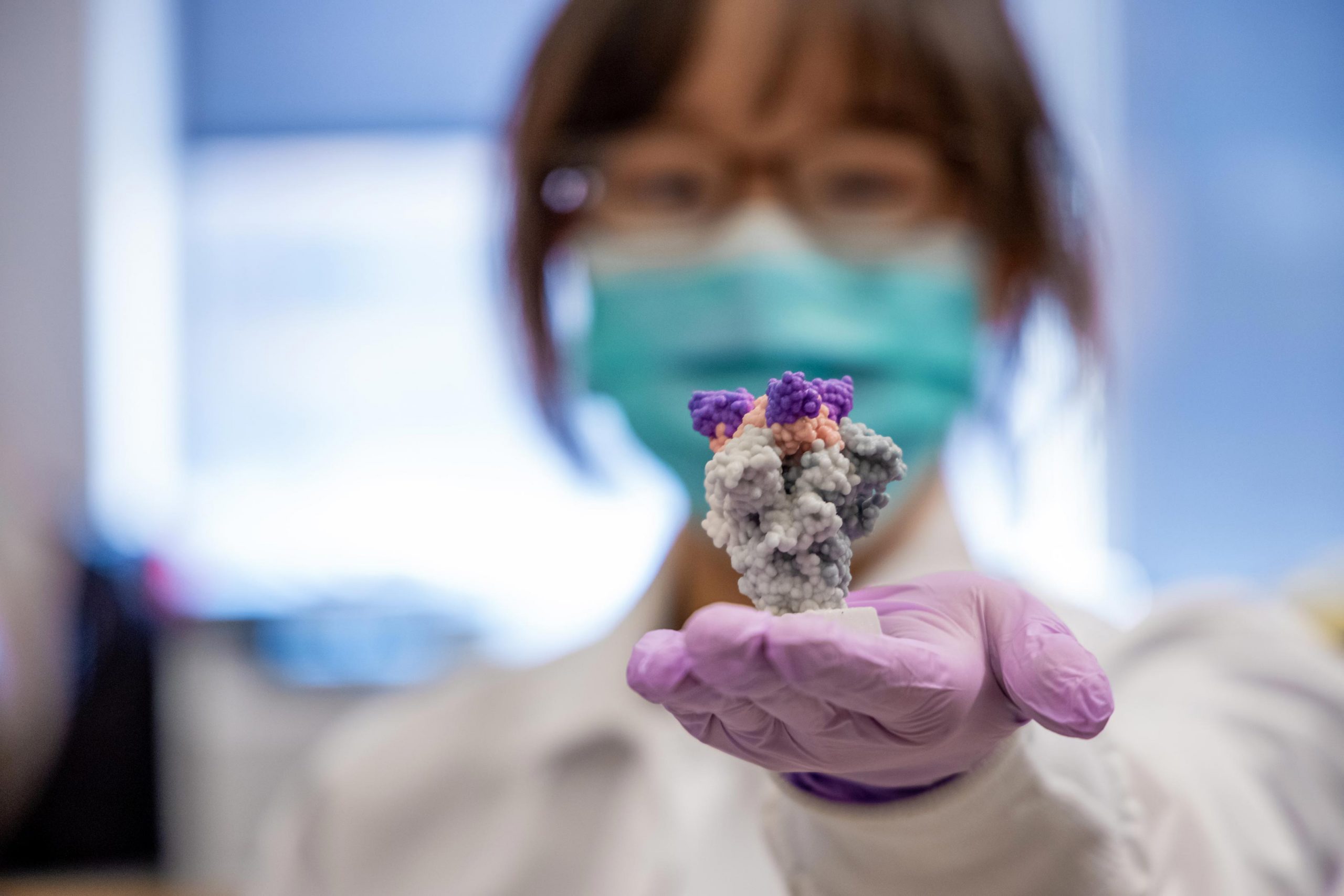
Lead author Yufei Xiang holds a 3D printed model of nanobodies (purple) above the SARS-CoV-2 spike protein (gray). Credit: UPMC
Researchers from the University of Pittsburgh School of Medicine describe in the journal Science, a new method to extract tiny but extremely powerful SARS-CoV-2 antibody fragments from llamas, which could be transformed into inhalable therapeutic agents with the potential to prevent and treat COVID-19[feminine.
Ces anticorps spéciaux de lama, appelés «nanocorps», sont beaucoup plus petits que les anticorps humains et beaucoup plus efficaces pour neutraliser le virus SARS-CoV-2. Ils sont également beaucoup plus stables.
«La nature est notre meilleur inventeur», a déclaré l’auteur principal Yi Shi, Ph.D., professeur adjoint de biologie cellulaire à Pitt. «La technologie que nous avons développée étudie les nanocorps neutralisant le SARS-CoV-2 à une échelle sans précédent, ce qui nous a permis de découvrir rapidement des milliers de nanobodies avec une affinité et une spécificité inégalées.
Pour générer ces nanocorps, Shi s’est tourné vers un lama noir nommé Wally – qui ressemble et partage donc son surnom avec le Labrador noir de Shi.
Dr Yi Shi, lead author of an article published in Science, explains how “nanobodies” could be a powerful new weapon against the COVID-19 pandemic. Credit: UPMC
Shi and his colleagues immunized the llama with a piece of the SARS-CoV-2 spike protein, and after about two months, the animal’s immune system produced mature nanobodies against the virus.
Using a mass spectrometry-based technique that Shi has been perfecting for three years, lead author Yufei Xiang, a research assistant in Shi’s lab, identified the nanobodies in Wally’s blood that bind most strongly to SARS. -CoV-2.
Then, with help from Pitt’s Vaccine Research Center (CVR), the scientists exposed their nanobodies to live SARS-CoV-2 virus and found that just a fraction of a nanogram could neutralize enough virus to prevent the infection of a million cells.

Wally the llama. Credit: Sonya Paske, Capralogics Ltd.
These nanobodies represent some of the most effective therapeutic antibody candidates for SARS-CoV-2, hundreds to thousands of times more effective than other llama nanobodies discovered through the same phage display methods used for decades to fish for human monoclonal antibodies.
Shi nanobodies can stay at room temperature for six weeks and tolerate being turned into an inhalable mist to deliver antiviral therapy directly to the lungs where they are needed most. Since SARS-CoV-2 is a respiratory virus, nanobodies could find it and attach itself to it in the respiratory system, before it even has a chance to cause damage.
In contrast, traditional anti-SARS-CoV-2 antibodies require an intravenous infusion, which dilutes the product throughout the body, requiring a much higher dose and costing patients and insurers about $ 100,000 per treatment.
“Nanobodies could potentially cost a lot less,” Shi said. “They are ideal for dealing with the urgency and scale of the current crisis.”
Together with Cheng Zhang, Ph.D., at Pitt, and Dina Schneidman-Duhovny, Ph.D., at the Hebrew University of Jerusalem, the team found that their nanobodies use a variety of mechanisms to block SARS. -CoV-2 infection. This makes the nanobodies ripe for bioengineering. For example, nanobodies that bind to different regions of the SARS-CoV-2 virus can be bound together, like a Swiss army knife, in case part of the virus mutates and becomes resistant to drugs.
“As a virologist, it’s amazing how harnessing the oddity of llama antibody generation can translate into the creation of a potent nanowear against clinical isolates of SARS-CoV-2,” he said. said study co-author and CVR director Paul Duprex, Ph.D.
Reference: “Polyvalent and multivalent nanobodies effectively neutralize SARS-CoV-2” by Yufei Xiang, Sham Nambulli, Zhengyun Xiao, Heng Liu, Zhe Sang, W. Paul Duprex, Dina Schneidman-Duhovny, Cheng Zhang and Yi Shi, 5 November 2020, Science.
DOI: 10.1126 / science.abe4747
Other study authors include Sham Nambulli, Ph.D., Zhengyun Xiao, Heng Liu, Ph.D., and Zhe Sang, all from Pitt.
Funding for this study was provided by the National Institutes of Health (grants R35GM137905 and R35GM128641), the Institute of Clinical and Translational Sciences at the University of Pittsburgh, the Pitt Center for Vaccine Research, and the DSF Charitable Foundation.
[ad_2]
Source link