[ad_1]
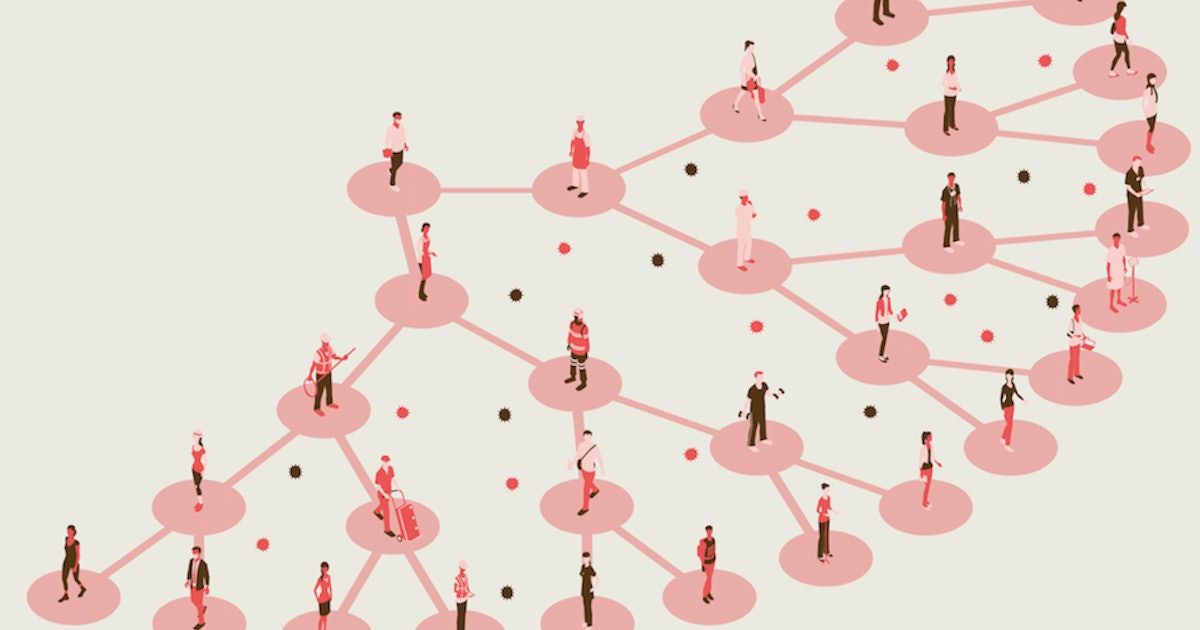
In recent history, no other world event radically transformed our daily movements just like Covid-19. To limit the insidious spread of the coronavirus, people have been advised to stay home, socially distanced and, at times, self-isolate.
To show how these mobility changes influence disease transmission, scientists have just published a large-scale, fine-grained dynamic model. The data shows how 98 million Americans in ten of the country’s largest metropolitan areas moved to half a million different establishments – from bodegas to wine bars to malls.
The data paints a sobering picture of what could happen if people abandon social distancing and return to normal lives in a fluctuating number of cases. But it also illuminates a future that does not require a total economic shutdown – if we choose a path associated with minimizing infections.
The findings, which offer critical insight to policymakers shaping public health policy, were published Tuesday in the journal Nature.
Instead of advising lockdown for months, the data identifies four “superspreader” sites who have the highest risk of infection:
Avoiding these establishments – if they are operating at full capacity – could save lives as people go through a cold, virus-laden winter, the study found.
“Without any reduction in mobility – without staying at home in a single month – 30% of the total population of these cities would be infected,” said study co-author Jure Leskovec, computer scientist at the University of Stanford, in a press appeal.
These infections occur very unevenly, Leskovec added: About 10% of the sites examined accounted for more than 80% of all infections. These places, on average, are smaller, more crowded, and are occupied for longer periods of time. Researchers predict that reducing foot traffic in these high-risk locations could have disproportionate positive effects on reducing infections.
“There is an important trade-off between wanting to restart the economy but also wanting to minimize the number of Covid cases,” Leskovec said.
“Our work demonstrates that it doesn’t have to be all or nothing.”
Study design – To determine how mobility patterns influence the spread of the coronavirus, the team used a massive set of cell phone data collected by SafeGraph, a company that aggregates anonymous location data from mobile apps.
Mobility data ranged from March 1 to May 2, 2020. It captures the hourly movements of people in local neighborhoods, technically referred to as groups of census blocks, each containing around 600 to 3,000 people.
Leskovec and his colleagues looked at three factors: where people go in a day, how long they linger in each place, and how many other people are visiting the same place at the same time.
They then built a computer model that takes into account the demographic origin of the people, the neighborhood in which they live and the daily density of each establishment. After running their simulation with multiple parameters, the team compared their predictions with the number of real-time confirmed coronavirus cases collected by The New York Times of the 10 metropolitan areas. These infections occurred between March 8 and May 9, 2020.
“The ability of our model to capture the true case curve, despite capturing only changes in mobility, suggests that mobility played a really important role in determining the infection curve,” said the co-author. of the study Serina Chang, researcher at Stanford University, during the call. .
Using this detailed model, the researchers say they can predict the likelihood of new infections occurring at a specific place or time, up to an hour.
Super-spreading sites and targeted occupation ceilings – While much attention has focused on the singular “super-spreaders” – individuals who inadvertently transmit the virus to large groups of people – these researchers have reversed that idea. Instead of looking at individual human super-spreaders, the team explored “super-spreading sites, “Places where the risk of transmission is dangerously high due to crowds or confined spaces.
The team confirmed that most transmissions of Covid-19 occur at four super-broadcaster sites: full-service restaurants, gyms, hotels and cafes. These places are especially risky because groups of people tend to stay nearby for long periods of time.
In Chicago, for example, only 10% of localities accounted for 85% of predicted infections.
Based on these findings, the team isn’t saying it’s necessary to shut down these places for months. Instead, policymakers should institute target occupancy ceilings to limit pedestrian traffic at each location.
The exact threshold would vary from city to city and community to community. Still, the team says reducing the occupancy rate to around 20-50 percent of capacity could significantly reduce the risk of catching or spreading the virus.
“It’s a particularly effective strategy because it targets points of interest during high-risk times,” Leskovec said. “With 20 percent occupancy, the restaurant still receives 60 percent of its visitors, but we’re preventing 80 percent of infections.”
In Chicago, the cap at 20% maximum occupancy predicted more than 80% new infections, but lost only 42% of all visits. The team saw similar trends in other cities.
The team also found that reopening some locations was riskier than others. In all of the cities in the study, full-service restaurants, gyms, hotels, cafes, religious organizations and limited-service restaurants produced the largest increases in infections expected when reopening.
Restaurants are by far the riskiest – by the way four times more risky than the following categories, which are gyms and cafes, followed by hotels, Leskovec said.
“The complete reopening of restaurants, after one month, would lead to the infection of about 6% of the total population,” he explained.
Who is most at risk – Just as various places are not affected equally in all areas, minority communities and low-income groups are also at disproportionate risk of transmission. Previous research associates these disparities with unequal access to health care and varying rates of pre-existing conditions.
This model suggests that mobility is a more important factor behind this disparity than previously assumed.
In the model, people living in low-income neighborhoods and less white neighborhoods were not able to reduce their mobility as much as high-income neighborhoods, possibly because they were essential workers or did not have not the luxury of working from home. In turn, these groups were significantly more likely to have been infected by the end of the simulation.
This predicted disparity was also due to frequentation of restaurants and full-service establishments which tended to be smaller and more crowded. Scientists have seen the same disparity manifest in neighborhoods with fewer whites.
The reopenings have also not affected communities in the same way. In Chicago, researchers predicted that fully reopening would infect an additional 39% of populations in low-income neighborhoods within a month, compared to 32% of the total population.
What happens after? – Based on this comprehensive analysis, the team also presented five targeted policy interventions that could make a significant difference in reigning in the spread of Covid-19:
- Stricter limits on the capacity of establishments.
- Emergency food distribution centers that can reduce foot traffic in high risk stores.
- Free and widely available tests in areas predicted to be high risk (especially given the known disparities in access to tests).
- Improved paid vacation policy or income support that allows essential workers to reduce mobility and stay home when sick.
- Improved infection prevention in the workplace for essential workers, including high quality PPE, good ventilation, and separation where possible.
These precautions can limit another catastrophic transmission and prevent cities from locking up.
Abstract: The COVID-19 pandemic has radically changed patterns of human mobility, requiring epidemiological models that capture the effects of changes in mobility on the spread of the virus. We introduce a metapopulation SEIR model that integrates fine-grained dynamic mobility networks to simulate the spread of SARS-CoV-2 in 10 of the largest metropolitan statistical areas in the United States. Derived from mobile phone data, our mobility networks map the hourly trips of 98 million people from neighborhoods (groups of census blocks or GBCs) to points of interest (POI) such as restaurants and religious establishments, connecting 57k GBC to 553k POI with 5.4 billion hourly edges. We show that by integrating these networks, a relatively simple SEIR model can precisely fit the trajectory of the real case, despite substantial changes in population behavior over time. Our model predicts that a small minority of “super-prevalent” POIs account for a large majority of infections and that restricting maximum occupancy at each POI is more effective than uniformly reducing mobility. Our model also correctly predicts higher infection rates among disadvantaged racial and socio-economic groups2–8 solely because of differences in mobility: we find that disadvantaged groups have not been able to reduce mobility as strongly and that the POIs they visit are more congested and therefore higher. risk. By capturing who is infected where, our model supports detailed analyzes that can inform more effective and fair policy responses to COVID-19.
[ad_2]
Source link