[ad_1]
By Nancy Lapid
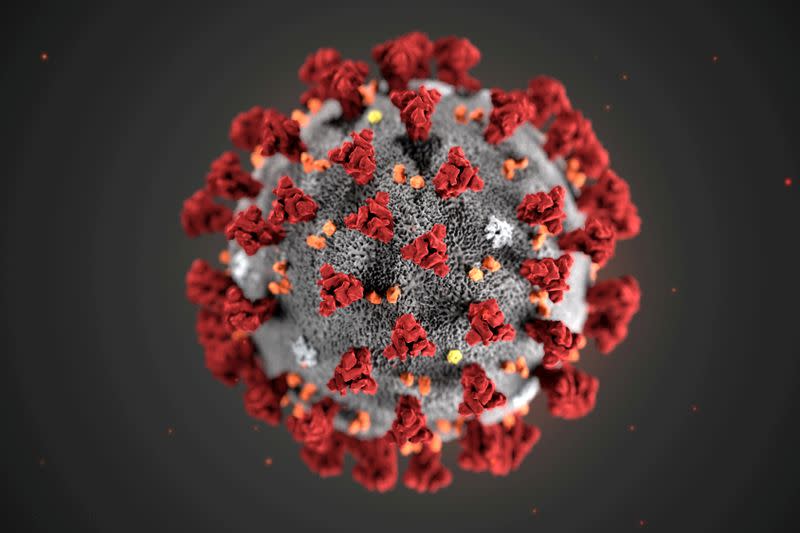
(Reuters) – The following is a summary of some of the latest scientific studies on the novel coronavirus and efforts to find treatments and vaccines for COVID-19, the disease caused by the virus.
Gut bacteria linked to severity of COVID-19, immune response
Microscopic organisms living in our intestines can influence the severity of COVID-19 and the body’s immune response to it, and could explain persistent symptoms, researchers reported in the journal Gut on Monday. They found that the intestinal microorganisms in patients with COVID-19 were very different from those in uninfected individuals. “COVID patients lack certain good bacteria known to regulate our immune system,” said Dr Siew Ng of the Chinese University of Hong Kong. The presence of an abnormal assortment of gut bacteria, or “dysbiosis,” persists after the virus has cleared and could play a role in the lingering symptoms that affect some patients, she said. His team has developed an oral formula of living bacteria called probiotics and a special capsule to protect organisms until they reach the intestine. “Compared to patients receiving standard care, our pilot clinical study showed that more COVID patients who received our microbiome immunity formula achieved complete resolution of symptoms,” Ng said, adding that those who received it had dramatically reduced markers of inflammation in their blood, a favorable increase in bacteria in their stools and they developed neutralizing antibodies against the virus. (https://bit.ly/3q9u1hb)
Pandemic harms mental health of ICU workers
Nearly half of the staff working in intensive care units (ICUs) in England suffer from severe anxiety, depression or post-traumatic stress disorder, with the feeling that it would be better to die, reported Wednesday researchers in Occupational Medicine. The study was conducted in June and July – before Britain began to experience its latest wave of hospitalizations. Among more than 700 healthcare workers in nine ICUs, 45% reached the probable clinical significance level for at least one of the four serious mental health disorders: severe depression (6%), PTSD (40%), severe anxiety ( 11%) or alcohol consumption problem (7%). More than one in eight reported frequent thoughts of harming or killing themselves in the past two weeks. The poor mental health of intensive care staff caring for critically ill and dying COVID-19 patients affects not only their quality of life, but also their ability to work effectively, the researchers said. The results show the urgent need for mental health services to be quickly accessible to all health workers. (https://bit.ly/2LN5SOQ; https://reut.rs/38GlzAn)
Cooling vests help COVID-19 nurses tolerate PPE
COVID-19 nurses who wear cooling vests under their personal protective equipment (PPE) feel less overwhelmed by heat during their shifts, suggests a small study. Seventeen nurses wore a light cooling vest under their PPE on one day, and PPE only on another day. On both days, participants swallowed an electronic capsule that provides a continuous reading of core body temperature. The vests resulted in a slight improvement in body temperature, but a much larger improvement in the feeling of being too hot, researchers reported in the journal Temperature. Only 18% of nurses reported thermal discomfort and 35% a slightly hot thermal sensation at the end of the day with the vest. This compared to 81% and 94%, respectively, on the day without the vest. “PPE is known to induce heat stress, which increases fatigue and sensory discontent, and is known to interfere with effective decision-making,” said study co-author Thijs Eijsvogels from Radboud University Medical Center in the Netherlands. CoolOver vests made by Dutch company Inuteq are easy to disinfect and reactivate in a refrigerator, he said, and may extend work tolerance time and improve recovery for clinicians involved in COVID-19 care . (https://bit.ly/2K9sXe5)
Diabetes Increases Risk of COVID-19 for Black Patients
Black patients with type 1 diabetes (T1D) who are infected with the novel coronavirus face a particularly high risk of a life-threatening diabetes complication known as ketoacidosis, new data show. T1D usually develops in children or young adults and requires daily insulin to survive. Researchers studied 180 patients from across the United States with T1D and COVID-19, 31% of whom were black and 26% Hispanic. Black patients were almost four times more likely to develop diabetic ketoacidosis (DKA) than white patients, the researchers reported in The Journal of Clinical Endocrinology and Metabolism. Hispanics had a slightly higher risk than white patients. Blacks and Hispanics were much less likely to use newer diabetes technologies such as continuous blood sugar monitoring and insulin pumps, and had significantly poorer blood sugar control than white patients. This suggested that the higher risk was likely due to structural and systemic inequalities, co-author Dr Osagie Ebekozien of the nonprofit T1D Exchange in Boston told Reuters. Particularly during the pandemic, healthcare providers should screen T1D patients for socio-economic factors that increase their risk for diabetic ketoacidosis such as food insecurity, insulin affordability and access. to supplies for diabetes, the researchers said. (http://bit.ly/3hWJZs8)
Open https://tmsnrt.rs/3a5EyDh in an external browser for a Reuters graphic on vaccines and treatments in development.
(Reporting by Nancy Lapid and Megan Brooks; Editing by Bill Berkrot)
[ad_2]
Source link